Snapshot
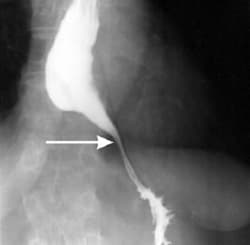
- A 41-year-old man presents to the clinic complaning of substernal chest pain and regurgitation of undigested food. He also reports having difficulty swallowing both solid and liquids. A barium esophgram demonstrates a dilated proximal esophagus with a narrow tapering.
Introduction
- Motor disorder of the distal esophagus secondary to progressive degeneration of the Aurbach plexus (ganglion cells in the myenteric plexus)
- Epidemiology
- incidence of 1.6 cases per 100,000 individuals
- demographics
- occurs equally among men and women
- diagnosis occurs between ages of 25 and 60 years
- risk factors
- Chagas disease
- other diseases such as scleroderma (see etiology)
- Etiology
- the etiology of primary/idiopathic achalasia is unknown
- Pathogenesis
- inflammation and degeneration of neurons of the Aurbach’s plexus
- the cause of the degeneration is unknown but may be autoimmune as suggested by the association with variants in the HLA-DQ regions in affected patients and the presence of antibodies to enteric neurons
- primarily leads to loss of nitric oxide-producing, inhibitory neurons that affect the relaxation of esophageal smooth muscle
- results in loss of normal relaxation of the lower esophageal sphincter (LES) and rise in basal sphincter pressure
- results in aperistalsis
- inflammation and degeneration of neurons of the Aurbach’s plexus
- Prognosis
- disease is progressive without treatment that ultimately leads to end-stage achalasia characterized by esophageal tortuosity, angulation, and megaesophagus (diameter >6 cm)
Presentation
- Symptoms
- dysphagia for solids and liquids
- regurgitation
- difficulty belching
- vomit
- heartburn/substernal chest pain
- weight loss
Imaging
- Radiography
- may demonstrate mediastinal widening
- Barium esophagram
- not a sensitive test for achalasia, as it may be interpreted as normal in up to 1/3 of patients
- positive findings include 1) dilation of the proximal esophagus 2) “bird-beak” appearance at the esophageal sphincter 3) aperistalsis 4) delayed emptying of barium
- Upper endoscopy
- may reveal dilated esophagus that contains residual material
- esophageal mucosa usually appears normal
- often performed after esophageal manometry to rule out malignancy
- Esophageal manometry
- gold standard – required to establish diagnosis
- high-resolution manometry (vs. conventional manometry) allows for categorization of the achalasia subtype, which can guide management
- findings include increased LES pressure, inability of the LES to relax, decreased peristalsis, and diffuse esophageal spasm
Differential
- Gastroesophageal reflux disease (GERD)
- distinguishing factor
- regurgitated food is typically sour tasting in GERD due to the presence of gastric acid
- will have nonspecific findings on manometry
- distinguishing factor
- Pseudoachalasia due to malignancy
- distinguishing factor
- may have the same manometry findings but can be differentiated from achalasia via upper endoscopy
- distinguishing factor
- Cardiovascular dysphagia
- distinguishing factor
- compression of the anterior esophagus by enlarged left atrium of the heart
- distinguishing factor
- normal manometry findings
Treatment
- Medical management
- Botulism toxin injections
- High initial success but have more frequent relapses and a shorter time to relapse compared to operative treatments
- often second-line therapy offered to patients who are high risk for complications
- pharmacological treatments (e.g., nifedipine, nitrates, or calcium channel blockers) are often ineffective and are limited by side effects
- indicated in patients who fail treatment with botulism toxin
- Botulism toxin injections
- Operative
- preferred option for patients who have average surgical risk though the efficacy of treatments decreases over time
- 1/3 to ½ of patients will require repeat treatment within 10 years
- endoscopic balloon dilation of LES
- Cure rate of 80%
- Complication of perforation in <3% of patients
- myotomy with fundoplication
- Similar outcomes to that of dilation
- peroral endoscopic myotomy (POEM)
- preferred option for patients who have average surgical risk though the efficacy of treatments decreases over time
- new endoscopic technique that allows for myotomy of more proximal esophageal muscle
Complications
- Esophageal carcinoma
- ↑ risk of esophageal squamous cell carcinoma secondary to chronic irritation from food stasis
- ulceration and bleeding


