Overview
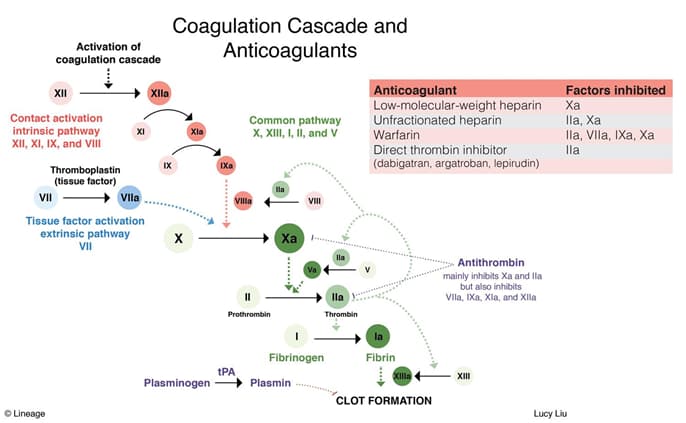
- Anticoagulants decrease the formation of fibrin clots
- heparin
- warfarin (coumadin)
- bivalirudin
Heparin
- Mechanism
- inactivates several factors
- IIa (thrombin)
- Xa
- IXa
- XIa
- XIIa
- inactivates several factors
- Clinical use
- immediate anticoagulation
- pulmonary embolism
- acute coronary syndrome
- stroke
- MI
- DVT
- DIC
- cardiovascular surgery
- during pregnancy
- does not cross placenta
- immediate anticoagulation
- Toxicity
- bleeding
- osteoporosis
- heparin-induced thrombocytopenia (HIT)
- heparin binds to platelet factor IV
- antibodies bind to and activate platelets
- leads to hypercoagulable state and thrombocytopenia
- hypersensitivity
- Pharmacology
- IV delivery only for therapeutic anticoagulation
- short half-life (2h)
- large, water-soluble polysaccharide
- low-molecular-weight heparins (e.g. enoxaparin) have advantages of
- longer half-lives (2-4x)
- less thrombocytopenia
- enhanced activity against factor Xa
- administered subcutaneously without laboratory (PTT) monitoring
- not easily reversible
- Monitoring
- partial thromboplastin time (PTT)
- Antagonist
- positively charged to bind negatively charged heparin
Warfarin (Coumadin)
- Mechanism
- ↓ hepatic synthesis of vitamin K-dependent clotting factors
- prevents the reduction of vitamin K, a necessary step in the synthesis of clotting factors
- affected clotting factors include
- II
- VII
- IX
- X
- protein C
- protein S
- no effect on clotting factors already present
- affects the extrinsic pathway
- ↓ hepatic synthesis of vitamin K-dependent clotting factors
- Clinical use
- chronic anticoagulation
- DVT prophylaxis
- post-STEMI
- heart valve damage
- atrial arrhythmias
- chronic anticoagulation
- Toxicity
- transient hypercoagulability
- transient protein C deficiency when beginning warfarin treatment
- due to short half life of protein C
- can lead to skin necrosis and dermal vascular thrombosis
- give heparin as you begin warfarin treatment
- transient protein C deficiency when beginning warfarin treatment
- bleeding
- teratogenic
- bone dysmorphogenesis
- not used in pregnancy
- drug interactions
- P450 metabolism
- inhibitors → ↑ PT
- decrease in P450 degrades less warfarin and levels rise
- mnemonics
- SICKFACES.COM
- Sodium valproate
- Isoniazid
- Cimetidine
- Ketoconazole
- Fluconazole
- Alcohol (binge drinking)
- Chloramphenicol
- Erythromycin
- Sulfonamides
- Ciprofloxacin
- Omeprazole
- Metronidazole
- SICKFACES.COM
- inducers → ↓ PT
- increase in P450 degrades more warfarin and levels fall
- mnemonics
- BS CRAP GPS “induces” rage
- Barbiturates
- St John’s Wort
- Carbamazepine
- Rifampin
- Alcohol (chronic)
- Phenytoin
- Griseofulvin
- Phenobarbital
- Sulfonylureas
- BS CRAP GPS “induces” rage
- inhibitors → ↑ PT
- ASA, sulfonamides, and phenytoin
- displace warfarin from plasma proteins, leading to increased free fraction → ↑ PT
- cholestyramine
- ↓ oral absorption
- due to low pKa
- ↓ oral absorption
- P450 metabolism
- transient hypercoagulability
- Pharmacology
- oral
- long half life (>30 hr)
- small, lipid-soluble
- Monitoring
- prothrombin time (PT)
- INR
- (tested PT / reference PT)^(calibration value)
- Antagonist
- vitamin K (slow onset)
- prothrombin complex concentrates (fast onset, low volume)
Lepirudin and Bivalirudin
- Mechanism
- direct inhibtors of thrombin (IIa)
- Clinical use
- unstable angina during percutaneous transluminal coronary angioplasty
Direct Factor Xa Inhibitors (Apixaban, Rivaroxaban, Edoxaban, and Betrixaban)



