Snapshot
- A five-year-old with severe asthma is being treated in the ER with a IV aminophylline drip. The child is slowly becoming sleepy and less responsive. Physical exam reveals less wheezing than on admission. Representative lung histology is shown.
- Definition
- episodic and reversible bronchoconstriction
- with bronchioles being the most susceptible respiratory segment
- result of
- inflammation
- bronchial smooth muscle hypertrophy and hyperactivity
- episodic and reversible bronchoconstriction
- mucus plugging
Classification
- Types
- extrinsic
- typically seen in children with a genetic predisposition
- type I hypersensitivty to an inhaled (external) allergen such as pollen
- proceeds by specific stages
- sensitization
- early activation
- mast cells are activated by cross-linking of IgE and release immune activating substances (histamine, leukotrienes, and acetylcholine) when allergen is presented again
- histamine results in bronchoconstriction, chemotaxis for immune cells, and mucus production
- acetylcholine results in bronchoconstriction (parasympathetic mediated)
- leukotrienes C4, D4, and E4 induce bronchoconstriction
- mast cells are activated by cross-linking of IgE and release immune activating substances (histamine, leukotrienes, and acetylcholine) when allergen is presented again
- proceeds by specific stages
- intrinsic
- non-allergen mediated
- induced by
- infection
- viral URI (RSV, rhinovirus, and parainfluenza virus)
- behavioral
- exertion and stress
- chemical
- drug sensitivity (NSAIDs and aspirin)
- ozone produced free-radicals
- infection
- status asthmaticus
- extrinsic
- life-threatening asthma attack that does not respond to standard treatments
Presentation
- Symptoms
- wheezing
- cough
- mucus production
- note: a child who is becoming sleepy and less responsive is most likely failing, retaining CO2 (case intro) and needs intubation
- Physical exam
- tachycardia
- tachypnea with use of accessory muscles
- result of reduced I/E ratio
- result of increased lung volume and vascular resistance
- auscultation
- prolonged expiratory wheezes (sometimes inspiratory)
- high pitched sibilant rhonchi
- dyspnea
- auscultation
- persistent cough with hyperinflation of the lungs
Imaging
- Chest radiograph
- normal or hyperinflation
Studies
- Labs
- ABG
- may initially show respiratory alkalosis
- if CO2 is normal, respiratory failure may be imminent
- elevated CO2 (respiratory acidosis) are ominous signs and patient likely requires intubation
- ABG
- Pulmonary function tests
- peak flows are diminished
- obstructive pattern may be seen when symptomatic (↓ FEV1/FVC)
- improvement with bronchodilator administration
- high airway resistance
- Methacholine challenge
- provacative measure of hyperactivity in a well patient
- functions as a muscarinic cholinergic agonist
- reduction of FEV1 by > 20% is diagnostic of asthma
- Skin testing
- may result in hypersensitivity response to allergen when presented into skin (really diagnoses atopy, not asthma)
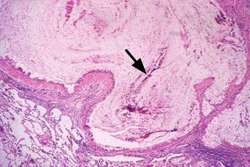
- Histological changes
- terminal bronchioles
- mucus plugs
- increased mucus-producing cells
- bronchi
- thickened basement membrane
- unique to asthma
- hypertrophy of submucosal glands and smooth muscle
- also seen in other lung disorders including chronic bronchitis
- thickened basement membrane
- terminal bronchioles
- increased immune cell presence
Treatment
- Acute exacerbation
- oxygen
- inhaled beta-2 agonists
- short acting preferred (e.g albuterol)
- appropriate for exercise induced asthma
- administer before exertion in known asthmatics
- systemic corticosteroids (PO or IV)
- Status asthmaticus
- oxygen, bronchodilators, and steroids
- sympathomimetic bronchodilators (e.g. epinephrine)
- intubation and mechanical ventilation
- Maintenance treatment
- inhaled corticosteroids (mainstay)
- long-acting bronchodilators (beta-2 agonists)
- in combintation with inhaled corticosteroids (increased risk of death if used without inhaled corticosteroid)
- montelukast
- cromolyn
- rarely used; supplemental treatment for exercise-induced asthma
- theophylline
- phosphodiesterase inhibitor; rarely used
- ipratropium bromide
- an anticholinergic that inhibits the contraction of smooth muscle
- used in the elderly with an asthmatic component to their COPD
- tiotropium
- more recently shown to be efficacious and safe


