Overview
Snapshot
- A 52-year-old man presents to his primary care physician with nocturia and increased day-time urinary frequency. He notices that he needs to strain when beginning to void and tends to dribble after he finishes urinating. Medical history is significant for hypertension treated with hydrochlorothiazide and type 2 diabetes mellitus treated with metformin. On digital rectal exam, there is a non-tender, smooth, elastic, and firm enlarged prostate. A urinalysis and prostate-specific antigen level is ordered.
Introduction
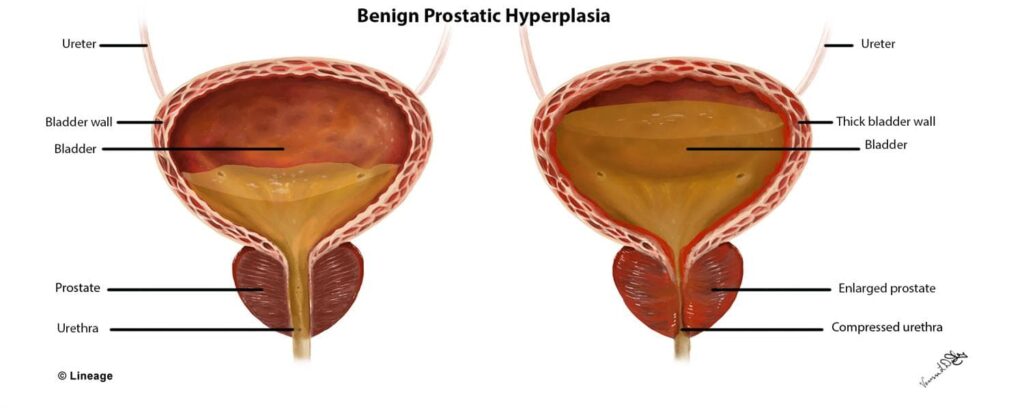
- Clinical definition
- benign hyperplasia of the stromal and epithelial cells of the prostate that results in lower urinary tract symptoms (LUTS) such as
- post-void dribbling
- increased urinary frequency and urgency
- nocturia
- weak urinary stream
- benign hyperplasia of the stromal and epithelial cells of the prostate that results in lower urinary tract symptoms (LUTS) such as
- Epidemiology
- demographics
- men > 45 years of age
- demographics
- Pathogenesis
- unclear; however, chronic inflammation and hormonal and vascular mechanisms may play a role
- Associated conditions
- obesity and metabolic syndromes
- hypertension
- type 2 diabetes mellitus
- Prognosis
- symptoms slowly and progressively worsen
Presentation
- Symptoms
- issues with urinary storage
- e.g., nocturia, increased urinary frequency, urinary incontinence, and urgency
- issues with voiding
- e.g., weak urinary stream, hesistancy, straining to void, and post-void dribbling
- irritative issues
- e.g., urgency and increased urinary frequency
- issues with urinary storage
- Physical exam
- digital rectal exam
- a non-tender, smooth, elastic, and firm enlarged prostate
Studies
- Labs
- urinalysis
- to detect the presence of a urinary tract infection or blood
- prostate-specific antigen
- non-specific
- urinalysis
- Diagnostic criteria
- this is a clinical diagnosis based on history (e.g., storage, voiding, and/or irritating urinary symptoms) and physical exam (e.g., a non-tender, smooth, elastic, and firm enlarged prostate)
Differential
Treatment
- Medical
- α1-blockers (e.g., terazosin and tamsulosin)
- indication
- considered initial therapy in patients with LUTS secondary to BPH
- results in immediate relief
- caution in patients on a phosphodiesterase-5 inhibitor as this can cause severe hypotension
- considered initial therapy in patients with LUTS secondary to BPH
- indication
- 5α-reductase inhibitors (e.g., finasteride)
- indication
- can be used as alternative treatment in patients with LUTS secondary to BPH who cannot tolerate α1-blockers
- takes time (6-12 months) for symptom improvement to be appreciated
- can be used as alternative treatment in patients with LUTS secondary to BPH who cannot tolerate α1-blockers
- indication
- phosphodiesterase-5 inhibitors (e.g., sildenafil)
- indication
- a reasonable treatment option in patients with LUTS secondary to BPH who have erectile dysfunction
- indication
- α1-blockers (e.g., terazosin and tamsulosin)
- Surgical
- transurethral resection of the prostate
- indication
- a treatment option in patients who are unresponsive to medical treatment
- indication
- transurethral resection of the prostate
- in patients with recurrent UTIs, bladder stones, or gross hematuria secondary to their BPH
Complications
- UTI
- Nephrolithiasis
- Bladder stones
- Chronic kidney disease


