Snapshot
- A 2-month-old boy presents with a 2-day history of fever and a painful bump on his rear-end. On exam, there is a fluctuant, erythematous bump with purulent material draining. The abscess is drained and cultured, and the patient is started on antibiotics. The cultures come back positive for S. aureus. This is his second episode of a S. aureus-induced abscess. A nitroblue tetrazolium test is negative.
Introduction
- Chronic granulomatous disease (CGD) is a rare primary immunodeficiency of phagocytes
- Genetics
- Epidemiology
- males > females due to inheritance pattern
- Pathogenesis
- recall normal physiology
- NADPH oxidase is important in respiratory or oxidative burst
- results in rapid release of reactive oxygen species such as superoxide
- recall normal physiology
- Leads to granulomas
Presentation
- Symptoms
- often appear in first year of life with recurrent pyogenic infections
- recurrent infection with catalase-positive organisms
- pneumonias
- aspergillosis
- skin abscesses
- pulmonary abscesses
- chronic diarrhea
- failure to thrive
- Physical exam
- short stature
- eczematoid dermatitis
- hepatomegaly
Evaluation
- Flow cytometry reduction of dihydrorhodamine
- abnormal
- can detect X-linked carrier status
- cannot differentiate oxidase-positive from oxidase-negative phagocyte subpopulations in CGD carriers
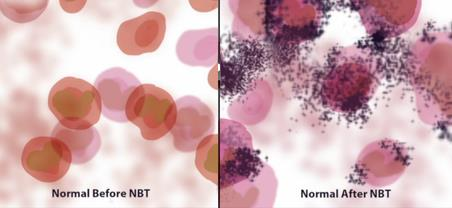
- Nitroblue tetrazolium dye reduction test
- negative finding = incubated leukocytes do not turn the plate blue
- Cytochrome c reduction assay
- measures production of reactive oxygen species
Differential Diagnosis
Treatment
- INF-γ
- Antibacterial and antifungal prophylaxis
- Only curative therapy
- hematopoietic stem cell transplant
Prognosis, Prevention, and Complications
- Prognosis
- improving with treatment
- 50% survival rate to age 30-40
- Prevention
- antifungals and antibiotics
- Complications
- severe fungal infections are often determinant of survival


