Snapshot
- A 70-year-old Caucasian man sees his primary care physician for his annual physical and labs. He has no complaints, and his physical exam is normal. His only medical problems are hypertension, managed with medication, and hyperlipidemia, controlled with diet. A few days later, his physician is concerned, noting that his WBC count is 30,000/μL with 90% lymphocytes. Peripheral blood smear shows smudge cells. He calls the patient in for further testing.
Introduction
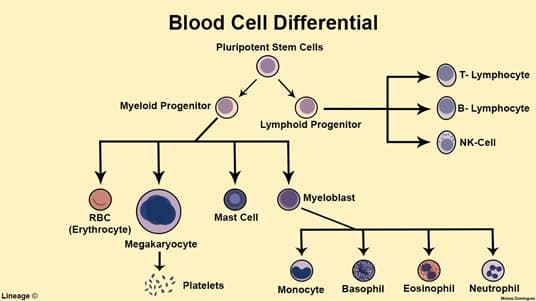
- Clonal proliferation of incompetent B-cells
- Epidemiology
- > 60 years of age
- most common form of leukemia in adults in Western countries
- more common in Caucasian males
- Many are diagnosed incidentally with markedly elevated WBC
- Insidious onset of symptoms (chronic, not acute)
- Associated conditions
- warm autoimmune hemolytic anemia (IgG)
Presentation
- Symptoms
- many are asymptomatic at presentation
- most common symptom is fatigue
- recurring infections
- Physical exam
- painful lymphadenopathy
- called small lymphocytic lymphoma when there is high degree of lymph node involvement and fewer cells in circulation
- painful lymphadenopathy
- hepatosplenomegaly
Evaluation
- Most accurate test
- flow cytometry – CD5, CD19, CD20, and CD23+ B-cells
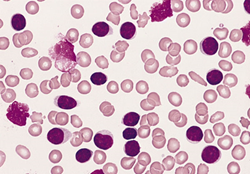
- Peripheral blood smear
- artifact of lab, from cover slip crushing the nucleus
Differential Diagnosis
Treatment
- Treatment only for symptomatic or rapid progression
- fludarabine – first-line
- ibrutinib – targeted against Bruton’s tyrosine kinase (BTK)
- alemtuzumab – antibody directed against CD52
- rituximab – antibody directed against CD20
- Curative therapy
- allogeneic stem cell transplant
Prognosis, Prevention, and Complications
- Prognosis
- most live 5-10 years after diagnosis
- some die rapidly, within 2-3 years
- Complications
- Richter syndrome/transformation
- transformation of CLL into aggressive large B-cell lymphoma
- 3-10% of cases
- weight loss, fevers, night sweats, cachexia, and lymphadenopathy
- poor prognosis
- Richter syndrome/transformation


