Snapshot
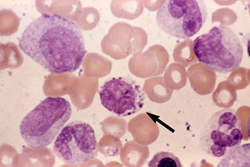
- A 62-year-old man presents to his primary care provider for an urgent care visit. He reports feeling very fatigued recently. He denies any change in bowel movements or any blood in his stool. On physical exam, he has mild splenomegaly. Blood tests come back with increased leukocytosis with neutrophilic dominance and increased basophils. Concerned, his primary care provider refers him to hematology-oncology. His peripheral smear shows myeloid cells.
Introduction
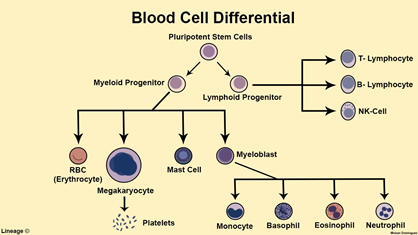
- Also known as chronic myelogenous leukemia
- Clonal hematopoietic stem cell disorder
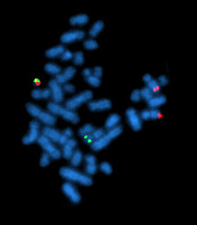
- Pathogenesis
- Philadelphia chromosome
- translocation t(9;22)
- BCR-ABL fusion gene
- hyperactive tyrosine kinase
- Epidemiology
- median disease onset 67 years of age
- 15% of all adult leukemias
- May transform into blast crisis
- AML or ALL
Presentation
- Symptoms
- B symptoms (fever, weight loss, fatigue)
- splenomegaly
- LUQ discomfort
- early satiety
- Physical exam
- splenomegaly common
Evaluation
- Complete blood count with differential
- ↑ WBC
- ↑ neutrophils
- ↑ basophils
- ↑ metamyelocytes
- ↓ leukocyte alkaline phosphatase
- low activity in mature granulocytes
- Bone marrow aspirate and biopsy
- Cytogenetic analysis or FISH showing Philadelphia chromosome (most accurate)
Differential Diagnosis
- Chronic myelomonocytic leukemia
- Chronic eosinophilic leukemia
- Primary myelofibrosis
- Acute myeloid leukemic
- Leukemoid reaction
- ↑ WBC
- ↑ leukocyte alkaline phosphatase
Treatment
- Medical management
- tyrosine kinase inhibitors are first-line
- imatinib (Gleevec)
- nilotinib
- dasatinib
- tyrosine kinase inhibitors are first-line
- Surgical management
- hematopoietic stem cell transplant
- never first-line
- hematopoietic stem cell transplant
- the only curative therapy
Prognosis, Prevention, and Complications
- Prognosis
- worse prognosis with older age at diagnosis
- increased overall survival with tyrosine kinase inhibitor therapy
- Complications
- transformation to acute leukemia (blast crisis)
- infection
- bleeding
- bone pain
- splenic infarcts due to splenomegaly



