Compartment Syndrome – Clinical Vignette
- A 21-year-old man presents to the emergency department with severe pain and swelling in his right leg. He reports that he had recently sustained a tibial fracture and had a tightly bound cast placed on his leg. He has been experiencing excruciating pain since the cast was removed, and the pain is exacerbated when the muscles underneath are palpated. On physical examination, his right leg is swollen and tender to palpation. The patient has a high intracompartmental pressure of 40 mmHg and a surgical consult is immediately called for further management.
Introduction – Compartment Syndrome
- Clinical definition – Compartment Syndrome
- a painful medical/surgical emergency condition that occurs when the tissue pressure inside an anatomical compartment, bound by fascia, exceeds the perfusion pressure, resulting in ischemia and necrosis.
- Epidemiology – Compartment Syndrome
- location
- Can occur in any compartment of the body but is most common in the legs >> and arms.
- risk factors
- Severe trauma: Long bone fracture, crush injury.
- Prolonged extremity ischemia with reperfusion.
- Spontaneous bleeding, hematoma.
- Burn injury, massive fluid resuscitation, SIRS.
- location
- Etiology
- the most common cause is a fracture
- tibia fracture
- soft tissue injury
- circumferential burns
- crush injuries
- constrictive dressing (e.g., splints, casts, or poor surgical positioning)
- penetrating wounds
- the most common cause is a fracture
- Pathogenesis
- blood flow is blocked when the tissue pressure exceeds the perfusion pressure within a fixed-volume compartment
- this results in a lack of oxygen and the accumulation of waste products, causing pain and decreased peripheral sensation
- irreversible tissue damage occurs between 6-8 hours after onset
- Prognosis
- higher chance of regaining function of the affected limb if a fasciotomy is performed within 12 hours
Presentation
- Symptoms
- Significant extremity pain is the primary feature; pain can be “out of proportion” to an apparent injury.
- Pain and other features can progress rapidly over a few hours.
- Tense, firm compartment (note: deep posterior compartment of the leg cannot be palpated).
- Pain is exacerbated by a passive stretch of muscle within the compartment.
- Compartment-specific neurovascular findings (eg, paresthesias, reduced sensation, muscle weakness, diminished pulses).
- Physical exam
- Physical examination alone has limited sensitivity and specificity for ACS. Serial examinations are important in patients at risk.
- firm, swollen, and wooden feeling of the muscles on palpation
- may have skin findings such as bullae
- ↓ vibration sensation
- ↓ 2-point discrimination
- 6 P’s are classically associated with compartment syndrome
- Pallor
- Pain out of proportion
- worse with passive stretch
- Paresthesia
- “pins and needles” sensation
- Pulselessness
- Poikilothermia
- Paralysis
- late finding
Imaging
- Radiography
- indication
- typically not needed for diagnosing compartment syndrome, but useful for characterizing any trauma such as fractures
- indication
Studies
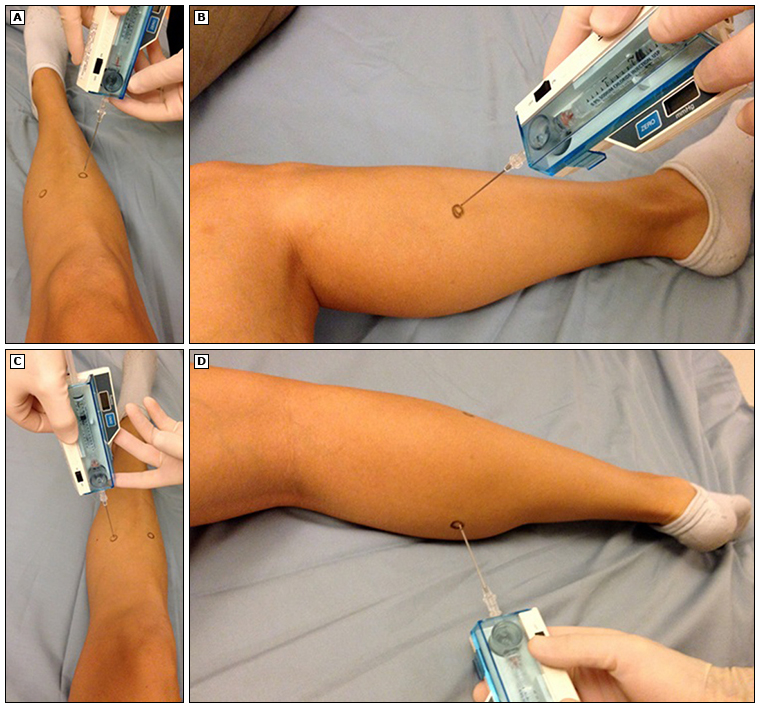
- Compartment pressure measurement
- indication
- to confirm the diagnosis if clinicians are unable to elicit the symptoms or history
- modality
- a transducer is connected to a catheter and is used to measure intracompartmental pressure (ICP)
- indication
- Making the diagnosis
- most cases of compartment syndrome are clinically diagnosed or guided by pressure measurement
- absolute ICP > 30 mm Hg
- Δ pressure (diastolic blood pressure – ICP) < 30 mmHg
- normal ICP = 0 mm Hg
- most cases of compartment syndrome are clinically diagnosed or guided by pressure measurement
Differential
- Cellulitis
- distinguishing factor
- normal neurovascular exam
- distinguishing factor
- Rhabdomyolysis
- distinguishing factors
- abnormal laboratory evaluation, including creatine phosphokinase, renal function studies, urine myoglobin, and potassium
- distinguishing factors
Treatment
- Management approach
- management of compartment syndrome is focused on early decompression
- observation and conservative management is appropriate only if ICPs are not high
- Conservative
- place the limb at the level of the heart without elevation
- indication
- for all patients while awaiting the diagnosis or decompression
- indication
- immediate removal of any wraps, splints, or casts
- indication
- for all patients
- indication
- immobilization
- indication
- for all patients
- indication
- place the limb at the level of the heart without elevation
- Operative treatments for compartment syndrome
- fasciotomy
- Extremity fasciotomy is the only recognized treatment for compartment syndrome. Early fasciotomy (ideally within four hours of symptom onset) can save the extremity.
- Indications:
- High clinical suspicion.
- Compartment pressure within 30 mmHg of diastolic pressure.
- Contraindications:
- Established late compartment syndrome is not likely to benefit from fasciotomy. Tissue damage becomes irreversible 4 to 8 hours after compartment pressure has increased. Fasciotomy for established ACS after 6 hours of onset increases the rate of infection and amputation.
- fasciotomy
Complications
- Volkmann contracture
- permanent nerve and muscle damage
- Rhabdomyolysis
- may occur with muscle ischemia, resulting in myoglobinuria and possible renal failure necessitating dialysis
Check out the USMLE STEP 1 COURSE.



