Introduction
- The complement system is a group of circulating proteins that
- are synthesized by the liver
- participate in humoral immunity
- act as proteases and cleave one another in cascade
- bind to pathogens as well as immune complexes
- alert phagocytes of the innate immune system
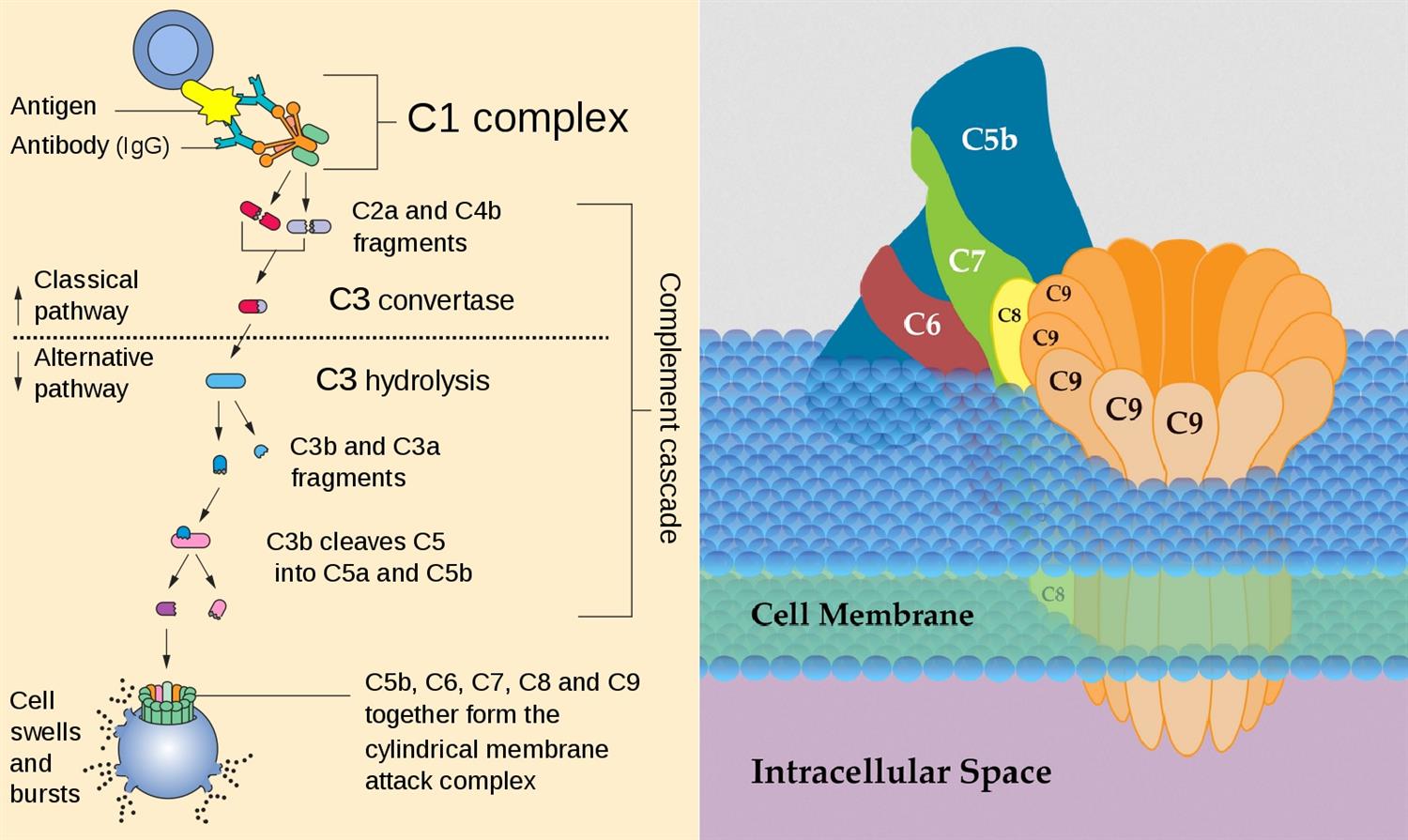
- The system can be activated in one of three ways including
- the classical pathway
- when activated by antibodies
- the alternative pathway
- when activated spontaneously
- the lectin pathway when
- activated by mannose residues on pathogens
- the classical pathway
- Activation of the complement pathway leads to
- a cascading cleavage of downstream proteins
- seperation of protein fragments after cleavage where
- a is the smaller component that is carried by the bloodstream
- b is the larger component that stays on the pathogen
- Complement must be closely controlled by inhibitors such as
- C1 esterase inhibitor
- CD55 (decay accelerating factor)
Activation of Complement SYstem
Functions
- The complement cascade has many functions including
- opsonization of invading pathogens mediated by
- coating of pathogens by C3b and IgG
- activation of phagocytosis by these fragments
- clearance of immune complexes and cellular debris
- chemotaxis of neutrophils mediated by
- release of C5a into bloodstream after cleavage
- detection of C5a by innate immune cells
- direct cytolysis of pathogens through
- formation of the membrane attack complex (MAC)
- insertion of the MAC into bacterial membranes
- rupture of the cell with release of internal contents
- vascular changes such as dilation that
- are caused by immune reaction to C3a, C4a, and C5a
- can lead to anaphylaxis if released systemically
- opsonization of invading pathogens mediated by
- Together these effects of the complement cascade are important in
- initial activation of the innate immune system
- clearance of debris such as immune complexes
- assistance with humoral immunity
Complement Component Deficiencies
Types:
The complement system consists of over 30 proteins, including:
- Serum Complement Proteins: These are present in the bloodstream and are typically inactive until they are triggered by an infection or inflammation.
- Cell-Bound Complement Proteins: Some complement proteins are found on the surface of immune cells, where they help in recognition and clearance of pathogens.
Function:
The complement system serves several crucial functions:
- Opsonization: Complement proteins mark pathogens for phagocytosis by immune cells, enhancing the clearance of microbes.
- Inflammation: Activation of complement proteins leads to the recruitment of immune cells and the initiation of the inflammatory response.
- Cell Lysis: The complement membrane attack complex (MAC) can insert into the membranes of pathogens, leading to cell lysis.
- Clearance of Immune Complexes: The complement system helps clear immune complexes and cellular debris.
Studies:
- Protein Structures: Research focuses on understanding the structures and functions of complement proteins.
- Activation Pathways: Studies investigate the different pathways (classical, lectin, and alternative) by which the complement system can be activated.
Clinical Significance:
- Infections: Deficiencies in the complement system can lead to an increased susceptibility to infections.
- Autoimmune Disorders: Overactivation of the complement system is implicated in several autoimmune diseases, including systemic lupus erythematosus (SLE) and rheumatoid arthritis.
Treatment Considerations:
- Complement Replacement Therapy: For individuals with complement deficiencies, complement replacement therapy may be considered to restore normal immune function.
- Immunosuppressive Drugs: In cases of complement-mediated autoimmune diseases, immunosuppressive drugs may be used to dampen the excessive immune response.
Future Directions:
- Therapeutic Targeting: Research explores the development of targeted therapies that can modulate complement activation, potentially improving outcomes in autoimmune diseases and transplant rejection.
- Complement in Infectious Diseases: Investigating the role of the complement system in various infections can lead to novel approaches for infection control.
Conclusion:
The complement system is a complex and critical component of the innate immune system, consisting of multiple proteins that work together to defend against infections and regulate inflammation. It serves functions ranging from opsonization and inflammation to cell lysis and immune complex clearance. Understanding the the is essential for diagnosing and managing complement deficiencies and complement-mediated diseases. Research into complement protein structures, activation pathways, and therapeutic targeting continues to expand our knowledge and may lead to innovative treatments in the future.
Check out USMLE Success Strategy: Personalized Consultation and Study Plan Development.


