Snapshot
- A 12 year old boy, previously healthy, is admitted to the hospital after 2 days of polyuria, polyphagia, nausea, vomiting and abdominal pain. Vital signs are: Temp 37C, BP 103/63 mmHg, HR 112, RR 30. Physical exam shows a lethargic boy. Labs are notable for WBC 16,000, Glucose 534, K 5.9, pH 7.13, PCO2 is 20 mmHg, PO2 is 90 mmHg.
Introduction
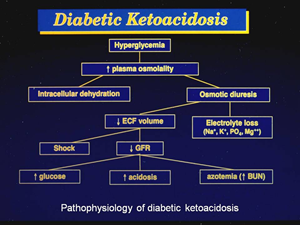
- Complication of type I diabetes
- result of ↓ insulin, ↑ glucagon, growth hormone, catecholamine
- Precipitated by
- infections
- MI
- drugs (steroids, thiazide diuretics)
- noncompliance
- pancreatitis
- undiagnosed DM
Presentation
- Symptoms
- abdominal pain
- vomiting
- Physical exam
- Kussmaul respiration
- increased tidal volume and rate as a result of metabolic acidosis
- fruity, acetone odor
- severe hypovolemia
- Kussmaul respiration
- coma
Evaluation
- Serology
- blood glucose levels > 250 mg/dL
- due to ↑ gluconeogenesis and glycogenolysis
- ↓ HCO3–
- consumed in an attempt to buffer the increased acid
- hyponatremia
- dilutional hyponatremia
- glucose acts as an osmotic agent and draws water from ICF to ECF
- dilutional hyponatremia
- moderate ketonuria and ketonemia
- due to ↑ lipolysis
- β-hydroxybutyrate > acetoacetate
- β-hydroxybutyrate not detected with normal ketone body tests
- hypertriglyceridemia
- due to ↓ in capillary lipoprotein lipase activity
- activated by insulin
- due to ↓ in capillary lipoprotein lipase activity
- leukocytosis
- due to stress-induced cortisol release
- blood glucose levels > 250 mg/dL
- H2PO4- is increased in urine, as it is titratable acid used to buffer the excess H+ that is being excreted
Treatment
- Fluids
- Insulin with glucose
- must prevent resultant hypokalemia and hypophosphatemia
- Long lasting insulin
- after the anion gap has closed during initial treatment
Prognosis, Prevention, and Complications
- 5-10% mortality
- Life-threatening mucormycosis
- thrive in ketoacidotic state
- Rhizopus infection
- Cerebral edema
- Cardiac arrhythmias
- due to electrolyte imbalances
- Heart failure
- due to hypovolemia



