Snapshot
- A 24-year-old woman presents to the ED with 6 hours of severe left lower quadrant abdominal pain and some moderate vaginal bleeding. She is sexually active with 1 male partner and uses condoms occasionally. She has a history of pelvic inflammatory disease. Her last period was 7 weeks ago. A transvaginal ultrasound is performed and shows a mass in the left adnexa.
Introduction
- Overview
- ectopic pregnancy is any pregnancy outside the uterine cavity
- ruptured ectopic is when the structure containing the pregnancy (such as fallopian tube) ruptures
- second leading cause of maternal mortality
- Epidemiology
- incidence
- 6-16% among women who present to ED with vaginal bleeding and/or pain
- estimated overall incidence 0.28-2.1% of pregnancies in U.S.
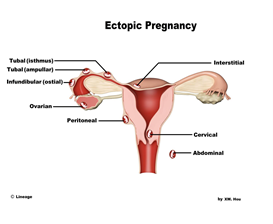
- location
- most commonly found in the fallopian tubes (96%)
- ampulla (75%)
- isthmus (12%)
- other sites
- abdomen
- hysterotomy scar (embedded in cesarean scar)
- cervix
- most commonly found in the fallopian tubes (96%)
- incidence
- Pathogenesis
- implantation of fertilized egg outside of the uterine cavity
- Prognosis
- life-threatening, if ruptured
- pregnancy is non-viable
Presentation
- History
- woman of reproductive age
- patient is sexually active
- missed recent period
- Symptoms
- usually present in first trimester
- 6-8 weeks after last normal menstrual period
- abdominal/pelvic pain
- may be sudden onset or slow onset
- no one typical type of pain: may be constant/intermittent, sharp/dull, and mild – severe
- referred shoulder pain may be present if rupture with sufficient blood to irritate diaphragm
- vaginal bleeding or spotting
- amenorrhea
- other symptoms of pregnancy
- breast tenderness
- frequent urination
- nausea
- temperature > 38°C is unusual (look for infectious cause)
- may be asymptomatic
- usually present in first trimester
- Physical exam
- cervical motion tenderness
- adnexal mass
- blood in vaginal canal
- ruptured ectopic pregnancy may present with
- hypotension
- signs of shock
- acute abdomen
Imaging
- Transvaginal ultrasound
- indications
- elevated β-hCG with no signs of uterine gestational sac on ultrasound is highly suspicious for ectopic
- assess for site of gestational sac with a yolk sac or embryo
- measuring the size will guide treatment
- findings
- peritoneal free fluid if ruptured
- if no mass visualized inside or outside uterus
- rely on serum β-hCG quantification (≥ 1500 mIU/mL or failure to double after 48 hours) to determine if ectopic
- “snowstorm” appearance of uterus indicates molar pregnancy
Studies
- Labs
- urine pregnancy test: positive
- serum β-hCG
- ≥ 1500 mIU/mL indicates ectopic pregnancy
- if < 1500 mIU/mL, repeat test in 48 hours
- in ectopic pregnancy β-hCG does not increase at an appropriate rate
- β-hCG level will be less than double after 48-72 hours
- intrauterine pregnancy: β-hCG will double after 48-72 hours
- Rh(D) typing and antibody screen
Differential
- Ruptured ovarian cyst
- negative β-hCG (unless ruptures during pregnancy)
- vaginal bleeding not usually associated
- pelvic ultrasound
- may see thin wall of previous cyst
- may see free fluid (also in ruptured ectopic)
- Molar pregnancy
- will see “snowstorm” appearance of uterus on ultrasound
- β-hCG may be much higher than in typical pregnancy or ectopic
- Spontaneous abortion
- intra-uterine pregnancy may be visualized on ultrasound
- cervical os may be open on pelvic exam
- may have passage of fetal contents from vagina
- β-hCG will decrease on 48-hour repeat test
Treatment
- Medical
- must meet the following criteria
- β-hCG ≤ 5000 mIU/mL
- gestational sac < 3.5 cm
- no fetal heart tone
- must meet the following criteria
- Surgical
- laparoscopic salpingostomy
- if does not meet criteria for medical management
- no signs of rupture
- laparoscopic salpingectomy
- if evidence of rupture
- free fluid in pelvic cavity
- signs of shock
- if evidence of rupture
- laparoscopic salpingostomy
- Follow up post-treatment β-hCG levels to ensure complete destruction of trophoblastic tissue
Complications
- Recurrent ectopic pregnancy
- incidence
- approximately 15%
- due to anatomic and functional changes in fallopian tubes secondary to clinical or subclinical salpignitis
- incidence
- Infertility
- incidence
- 11-62%
- risk factors
- prior history infertility
- pregnancy rate following ectopic pregnancy in women with history of infertility is one-fourth that of women without known infertility prior to ectopic
- decreased risk if ectopic occured during IUD use
- prior history infertility
- incidence
- Death
- incidence
- approximately 31.9 per 100,000 pregnancies
- risk factors
- ruptured ectopic pregnancy
- severe hemorrhage from intraperitoneal bleeding
- ruptured ectopic pregnancy
- incidence


