Overview (Fetal Circulation and Erythropoiesis)
- Umbilical vein
- returns 80% saturated blood from the placenta to the fetus
- Umbilical arteries
- carry mainly deoxygenated blood back to the placenta for oxygenation
- Erythropoeisis
- begins at week 3
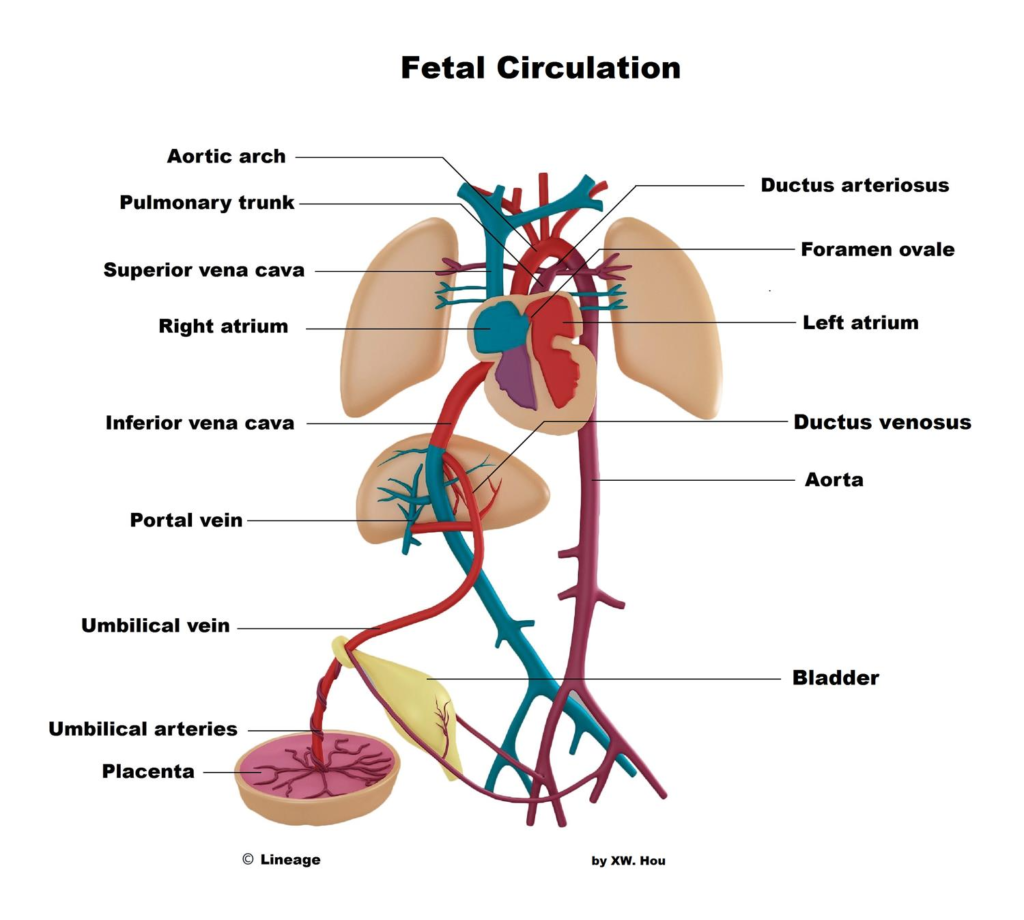
Circulatory Shunts
- Ductus venosus
- Foramen ovale
- due to the increased pulmonary resistance, oxygenated blood entering the right atrium is diverted from the lungs through the foramen ovale into the left atrium to deliver oxygenated blood to the body
- closes after birth due to increased left atrial pressure and becomes fossa ovalis
- Ductus arteriosus
- connects pulmonary artery to aortic arch
- deoxygenated blood that enters the right ventricle to be pumped through the pulmonary arteries is mostly diverted from the lungs to the body into the aortic arch via the ductus arteriosus
- becomes ligamentum arteriosum upon closure at birth
Infant’s first breath
- First breath
- pulmonary resistance ↓ causing ↓ in right atrial pressure
- ↑ venous return to left atria causes ↑ pressure resulting in the foramen ovale to close
- ↑ in O2 tension leads to ↓ in prostaglandin production resulting in closure of ductus arteriosus
- e.g., alprostadil is an PGE1
Fetal Erythropoiesis
- Hemoglobin
- composed of 2 sets of 2 subunits
- α2γ2 – fetal form
- α2β2 – adult form
- γ subunit has greater affinity than β subunit to allow for oxygen transfer across the placenta
- hemoglobin production
- week 3-8: yolk sac
- week 6-30: liver
- week 9-28: spleen
- composed of 2 sets of 2 subunits
- week 28: bone marrow
Introduction
Fetal circulation and erythropoiesis are two essential aspects of prenatal development that ensure the proper supply of oxygen and nutrients to the developing fetus. Fetal circulation allows for efficient gas exchange within the placenta, while erythropoiesis is the process of red blood cell formation in the fetus. Understanding these processes is critical for medical professionals, especially those in obstetrics, neonatology, and pediatric medicine. This article provides a comprehensive overview of fetal circulation and erythropoiesis, including their types, function, related studies, treatment considerations, and clinical significance.
Fetal Circulation:
Fetal circulation is unique and different from postnatal circulation. It is designed to facilitate efficient gas exchange in the placenta and bypass certain non-functional organs:
- Placenta: The placenta serves as the site of gas exchange, where oxygen and nutrients are delivered from the mother’s blood to the fetus, and carbon dioxide and waste products are transported from the fetus to the mother.
- Umbilical Cord: The umbilical cord connects the fetus to the placenta, providing a pathway for the exchange of blood and nutrients.
Types and Function of Fetal Circulation:
- Ductus Venosus: The ductus venosus is a vessel that shunts oxygenated blood from the umbilical vein directly to the inferior vena cava, bypassing the liver.
- Foramen Ovale: The foramen ovale is an opening between the atria of the fetal heart, allowing oxygenated blood from the right atrium to flow directly to the left atrium, bypassing the non-functional fetal lungs.
- Ductus Arteriosus: The ductus arteriosus is a vessel that shunts blood from the pulmonary artery to the aorta, directing blood away from the non-functional fetal lungs.
Clinical Significance:
- Patent Ductus Arteriosus (PDA): PDA is a condition where the ductus arteriosus fails to close after birth, leading to abnormal blood flow between the aorta and pulmonary artery. It may require medical or surgical intervention.
- Atrial Septal Defect (ASD): ASD is a congenital heart defect characterized by an abnormal opening between the atria, allowing blood to shunt from the left atrium to the right atrium. It can affect fetal circulation and may require treatment after birth.
Fetal Circulation Studies:
- Prenatal Ultrasound: Prenatal ultrasound is a valuable tool for assessing fetal circulation and identifying any abnormalities or potential complications during pregnancy.
Erythropoiesis in Fetal Development:
Erythropoiesis is the process of red blood cell (RBC) formation. During fetal development, erythropoiesis occurs in various sites at different stages:
- Yolk Sac: In the early stages of embryonic development (weeks 3-8), the yolk sac is the primary site of erythropoiesis, producing primitive RBCs.
- Liver: As gestation progresses, the liver becomes the main site of erythropoiesis during the second trimester.
- Bone Marrow: In the third trimester and after birth, the bone marrow gradually takes over as the primary site of erythropoiesis.
Erythropoiesis Function and Hemoglobin Switch:
- Hemoglobin F (HbF): During fetal development, the predominant type of hemoglobin is hemoglobin F (HbF), which has a higher affinity for oxygen than adult hemoglobin (HbA). This allows efficient oxygen transfer across the placenta.
- Hemoglobin Switch: After birth, there is a gradual transition from HbF to HbA, which becomes the predominant hemoglobin type in adulthood.
Clinical Significance:
- Hemolytic Disease of the Newborn (HDN): HDN can occur when maternal antibodies cross the placenta and attack fetal RBCs, leading to hemolysis. Rhesus (Rh) incompatibility is a common cause of HDN.
Erythropoiesis Studies:
- Hemoglobin Electrophoresis: This test is used to analyze the different types of hemoglobin present in the blood, helping to diagnose various hemoglobinopathies.
Treatment Considerations:
- Rhesus (Rh) Immunoglobulin: Rhesus immunoglobulin is administered to Rh-negative pregnant women to prevent the formation of antibodies against Rh-positive fetal RBCs and reduce the risk of HDN.
- Blood Transfusion: In severe cases of HDN or other fetal anemias, intrauterine or postnatal blood transfusions may be necessary to address anemia and ensure proper oxygen delivery.
Conclusion:
Fetal circulation and erythropoiesis are vital processes in prenatal development, ensuring proper oxygen and nutrient supply to the developing fetus. Understanding fetal circulation allows for the detection of potential anomalies or disorders that may require medical intervention after birth.
Check out Ultimate USMLE Step 1 Study Notes.


