Snapshot
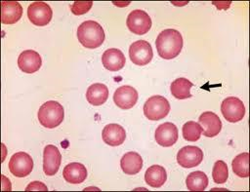
- A 25-year-old man with Mediterranean ancestry presents with jaundice. He also reports being unusually tired and believes this may be due to his recent recovery from mononucleosis. He was found to be anemic with a hemoglobin of 9 g/dL. His peripheral blood smear revealed bite cells and Heinz bodies.
Introduction
- Clinical definition
- glucose-6-phosphate dehydrogenase (G6PD) deficiency is an X-linked genetic disorder that causes an intrinsic hemolytic anemia
- Epidemiology
- prevalence
- 7.1% worldwide
- most common enzyme disorder of erythrocytes
- demographics
- more severe in males than females
- common in areas where malaria is endemic
- sub-Saharan Africa
- Middle East
- southeast Asia
- Mediterranean regions
- Pacific islands
- prevalence
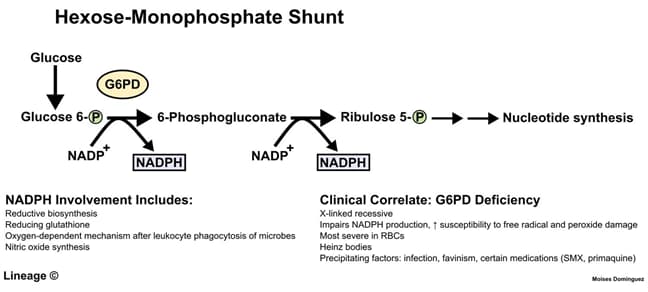
- Pathophysiology
- G6PD affects the pentose phosphate (hexose monophosphate) pathway
- this pathway generates nicotinamide dinucleotide phosphate (NADPH), which protects red blood cells against oxidative stress
- in red blood cells (without mitochondria), this pathway is the only source of NADPH
- acute hemolytic anemia following exposure to oxidative stressors
- primaquine
- dapsone
- sulfa drugs
- infections
- fava bean ingestion
- oxidative stressors cause
- G6PD deficiency is thought to decrease risk of severe malaria
- G6PD affects the pentose phosphate (hexose monophosphate) pathway
- Genetics
- inheritance pattern
- X-linked
- inheritance pattern
- Prognosis
- natural history of disease
- typically asymptomatic until exposed to oxidative stressors
Presentation
- Symptoms
- primary symptoms
- neonatal hyperbilirubinemia on day 2-4
- acute hemolytic anemia following exposure to precipitants, typically within 24-72 hours after ingestion
- fatigue
- jaundice
- dark urine
- back pain
- primary symptoms
- Physical exam
- jaundice
Studies
- Labs
- complete blood count and reticulocyte count
- urine
- hemoglobinuria
- G6PD activity assays
- indication
- screening
- fluorescent spot test
- most sensitive
- methemoglobin reduction test
- indication
- Quantitative assays
- indications
- confirmation of diagnosis
- a normal G6PD level immediately after hemolysis does not rule out G6PD deficiency
- confirmation of diagnosis
- indications
- spectrophotometry analysis
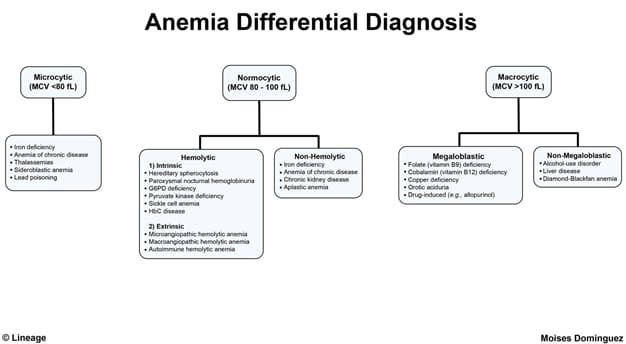
Differential
- Gilbert syndrome
- jaundice at birth (rather than delayed onset of jaundice)
- normal G6PD enzyme activity
- Hereditary spherocytosis
- spherocytosis seen on peripheral blood smear
Treatment
- Conservative
- avoid oxidative stressors
- Medical
- blood transfusion
- indication
- blood transfusion
- if severe
Complications
- Recurrence of acute hemolysis


