Overview
- Nicotinic antagonist (Ganglionic Blockers )
- hexamethonium
- first drug developed for hypertension treatment
- mecamylamine
- CNS penetration therefore can result in sedation, tremor, and choreiform movements
- trimethaphan
- short-acting, IV-administered
- hexamethonium
- Clinical use
- block nicotinic receptors at sympathetic and parasympathetic autonomic ganglia
- have low selectivity and wide array of effects limiting its use
- used in experimental models to prevent vagal reflex responses to changes in blood pressure such as to prevent reflex bradycardia caused by NE
- Toxicity
- severe orthostatic hypotension
- cycloplegia with loss of accommodation
- constipation
- sexual dysfunction: may prevent erection and ejaculation
- urinary retention in men with prostatic hyperplasia
Ganglionic Blockers
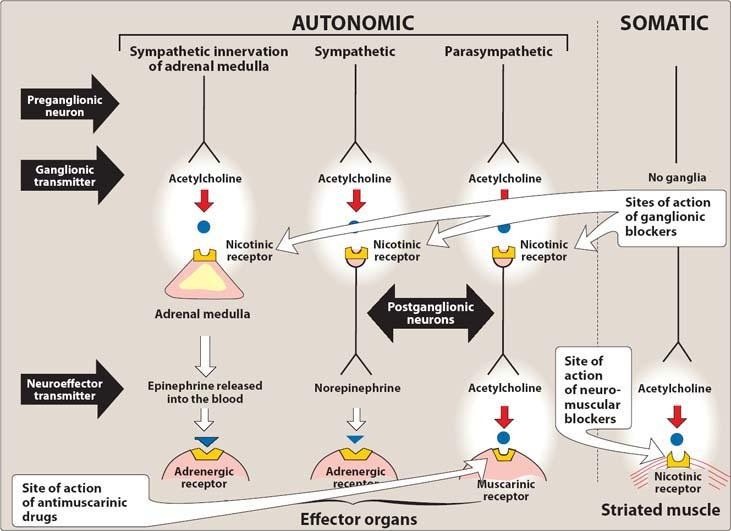
Ganglionic blockers, also known as ganglionic blocking agents, are a class of medications that inhibit the transmission of signals in the autonomic ganglia. Autonomic ganglia are clusters of nerve cells that play a crucial role in the transmission of impulses between the central nervous system and peripheral tissues.
Here’s an overview:
Mechanism of Action: It work by blocking the nicotinic acetylcholine receptors in autonomic ganglia. These receptors are responsible for transmitting signals between preganglionic and postganglionic neurons in the sympathetic and parasympathetic divisions of the autonomic nervous system. By blocking these receptors, ganglionic blockers inhibit the transmission of impulses, leading to a decrease in sympathetic and parasympathetic activity.
Effects on the Autonomic Nervous System:
- Sympathetic blockade: Ganglionic blockers reduce sympathetic outflow, resulting in decreased heart rate, decreased blood pressure, and peripheral vasodilation. This can lead to orthostatic hypotension (low blood pressure upon standing), reduced exercise tolerance, and impaired temperature regulation.
- Parasympathetic blockade: Ganglionic blockers can also block parasympathetic ganglia, resulting in symptoms such as dry mouth, urinary retention, constipation, and blurred vision.
Clinical Uses: Due to their non-selective and potent effects on autonomic ganglia, ganglionic blockers are rarely used in clinical practice. They were historically used to treat severe hypertension, but their use has significantly declined due to their adverse effects and the availability of more selective antihypertensive agents.
Adverse Effects:
- Hypotension: Ganglionic blockers can cause severe hypotension, especially when standing or during postural changes, which may lead to dizziness, fainting, or falls.
- Tachycardia: Reflex tachycardia can occur as a compensatory response to the decreased blood pressure.
- Gastrointestinal effects: Ganglionic blockers can cause constipation and impaired gastrointestinal motility.
- Urinary effects: Urinary retention is a common adverse effect due to the inhibition of parasympathetic ganglia involved in bladder function.
- Dry mouth: Ganglionic blockers can lead to decreased salivation, resulting in dry mouth.
- Ocular effects: Blurred vision and decreased accommodation may occur due to the inhibition of parasympathetic ganglia controlling pupillary constriction and lens accommodation.
Examples:
- Hexamethonium
- Mecamylamine
- Trimethaphan
It’s important to note that ganglionic blockers are not commonly used in contemporary medical practice due to their significant side effects and the availability of more selective and better-tolerated antihypertensive agents.
Studies
- Hypertension Treatment: Ganglionic blockers were historically used as antihypertensive agents. Several studies have investigated their efficacy in reducing blood pressure and managing hypertension. However, due to their significant side effects and the availability of more selective antihypertensive medications, ganglionic blockers are not commonly used as first-line therapy for hypertension.
- Autonomic Disorders: It have been studied in certain autonomic disorders characterized by dysregulation of sympathetic and parasympathetic activity. For example, they have been explored in conditions such as autonomic neuropathy, postural orthostatic tachycardia syndrome (POTS), and complex regional pain syndrome. However, their use in these conditions is limited and requires careful consideration due to the potential adverse effects.
- Experimental Research: Ganglionic blockers have been utilized in experimental research to understand the autonomic nervous system’s role in various physiological processes. They have been employed in studies investigating cardiovascular control, neural regulation of blood pressure, and autonomic reflexes.
- Adverse Effects and Tolerability: Research has focused on understanding and characterizing the adverse effects associated with ganglionic blockers. Studies have assessed their impact on blood pressure regulation, heart rate, gastrointestinal function, bladder function, and ocular effects. These investigations contribute to a better understanding of the tolerability and safety profiles of ganglionic blockers.
- Comparison Studies: Ganglionic blockers have been compared with other antihypertensive agents or treatment modalities to evaluate their relative efficacy and safety. These studies help assess the benefits and limitations of using ganglionic blockers in specific clinical scenarios compared to alternative therapeutic options.
Ganglionic blockers are a topic that can be tested in the pharmacology section of the USMLE. It is crucial for medical students to have a comprehensive understanding of the mechanism of action, clinical uses, adverse effects, and examples. Familiarity with the limited clinical use of these medications and the availability of alternative treatment options is important for answering related exam questions.
In summary, inhibit the transmission of signals in the autonomic ganglia by blocking nicotinic acetylcholine receptors. They have non-selective effects on the autonomic nervous system and were historically used as antihypertensive agents. However, their use has declined due to significant adverse effects and the availability of more targeted therapies. Understanding the key points about ganglionic blockers is important for medical students preparing for the USMLE pharmacology section.
Check out USMLE Step 1 Mastery: Comprehensive Course and Lecture Notes.


