Overview of Gastrointestinal Tract Histology
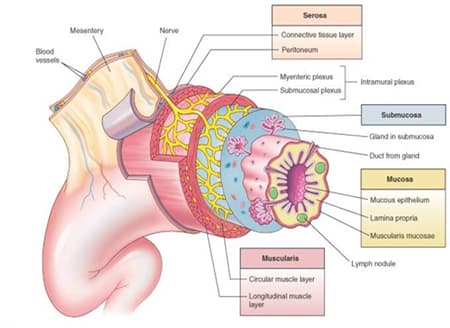
- Radial organization of gastrointestinal tract
- wall of tubular gastrointestinal tract consists of 4 concentric layers:
- mucosa
- epithelium
- typically a simple cuboidal or a simple columnar epithelium
- secretory function in stomach
- secretory and absorptive functions in small intestine and large intestine
- lamina propria
- supports avascular mucosal epithelium
- contains blood and lymphatic vessels
- supports avascular mucosal epithelium
- muscularis mucosae
- typically a double layer of smooth muscle
- inner layer of circularly oriented smooth muscle
- outer layer of longitudinally oriented smooth muscle
- contraction causes local movement in mucosa
- typically a double layer of smooth muscle
- epithelium
- submucosa
- a layer of connective tissue
- contains large blood vessels and large lymphatic vessels
- contains submucosal (Meisnner’s) nerve plexus
- anchors the mucosa to the muscularis externa
- muscularis externa
- a double layer of smooth muscle
- inner layer of circularly oriented smooth muscle
- outer layer of longitudinally oriented smooth muscle
- a double layer of smooth muscle
- contains myenteric (Auerbach’s) nerve plexus in between double layer of smooth muscle
- contraction causes peristalsis
- adventitia / serosa
- mucosa
- wall of tubular gastrointestinal tract consists of 4 concentric layers:
- a layer of connective tissue
Distinctive Features of Gastrointestinal Tract Histology
- Esophagus
- esophageal mucosa
- non-keratinizing, stratified squamous epithelium
- muscularis mucosae is a single layer of longitudinally oriented smooth muscle
- esophageal muscularis externa
- upper one third of esophagus
- striated muscle
- middle one third of esophagus
- striated muscle and smooth muscle
- lower one third of esophagus
- smooth muscle
- upper one third of esophagus
- esophageal mucosa
- Stomach
- gastric mucosa
- gastric glands occupy gastric mucosa
- simple, branched, tubular glands that extend from muscularis externa to bottom of gastric pits
- consist of mucus neck cells, parietal cells, chief cells, and G cells
- elaborate gastric secretions into lumen of stomach via gastric pits
- gastric glands occupy gastric mucosa
- gastric mucosa
- Small Intestine
- overview
- small intestinal mucosa
- exhibits numerous projections, or villi, that protrude from epithelial layer of mucosal surface
- villi increase surface area over which digestion and absorption occurs
- epithelial layer of small intestinal mucosa is heterogeneous, composed of:
- mucus-secreting cells (goblet cells)
- absorptive cells (enterocytes)
- exhibit numerous projections, or microvilli, that protrude from apical border
- microvilli increase surface area over which digestion and absorption occurs
- microvilli are responsible for characteristic striated border, or brush border, of enterocytes
- exhibit numerous projections, or microvilli, that protrude from apical border
- frequency of villi and of microvilli in small intestine
- jejunum > duodenum and ileum
- frequency of goblet cells in small intestine increases as you progress down the small intestine
- duodenum < jejunum < ileum
- exhibits numerous projections, or villi, that protrude from epithelial layer of mucosal surface
- small intestinal mucosa
- duodenum
- duodenal mucosa
- crypts of Lieberkühn, or intestinal glands, occupy duodenal mucosa
- simple tubular glands that extend from muscularis externa to base of villi
- elaborate small intestinal secretions into lumen of duodenum
- crypts of Lieberkühn, or intestinal glands, occupy duodenal mucosa
- duodenal mucosa
- jejunum
- jejunal mucosa
- crypts of Lieberkühn, or intestinal glands, occupy jejunal mucosa
- jejunal submucosa
- plicae circulares are circularly arranged transverse folds containing a core of submucosa that extend partially around jejunal lumen
- jejunal mucosa
- ileum
- ileal mucosa
- Peyer’s patches, or aggregations of nodules of unencapsulated lymphatic tissue, occupy ileal lamina propria (and ileal submucosa)
- M cells, overlying Peyer’s patches, function as antigen-transporting cells
- take up microorganisms and macromolecules
- deliver antigens to antigen-processing macrophages
- macrophages present processed antigen to lymphocytes
- triggers secretory immunity
- stimulates B cells in germinal centers of Peyer’s patches to differentiate into IgA-secreting plasma cells that reside in ileal lamina propria
- triggers secretory immunity
- macrophages present processed antigen to lymphocytes
- M cells, overlying Peyer’s patches, function as antigen-transporting cells
- crypts of Lieberkühn, or intestinal glands, occupy ileal mucosa
- Peyer’s patches, or aggregations of nodules of unencapsulated lymphatic tissue, occupy ileal lamina propria (and ileal submucosa)
- ileal submucosa
- plicae circulares are circularly arranged transverse folds containing a core of submucosa that extend partially around ileal lumen (proximal ileum)
- increase surface area over which absorption occurs
- plicae circulares are circularly arranged transverse folds containing a core of submucosa that extend partially around ileal lumen (proximal ileum)
- ileal mucosa
- overview
- Large intestine
- colon
- colonic mucosa
- “smooth” surface devoid of villi
- crypts of Lieberkühn, or intestinal glands, occupy colonic mucosa
- colonic mucosa
- anal canal
- anal canal mucosa
- keratinizing, stratified squamous epithelium
- anal canal mucosa
- colon



