- Week 1-6
- embryo is sexually indifferent
- genetically male and female embryos are phenotypically the same
- both male and female have mesonephric (Wolffian) ducts at this stage
- Week 7
- sexual differentiation occurs
- Week 12
- sex of embryo can be distinguished based on external genitalia
- Week 20
- phenotypical differentiation is complete
Male vs. Female Differentiation
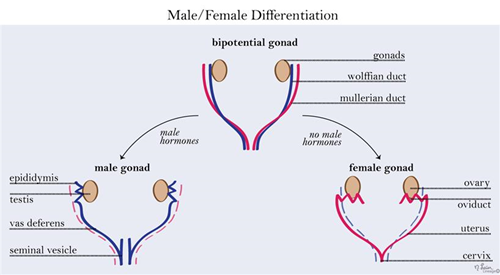
- Mesonephric (wolffian) duct
- needs to be induced to develop
- by testosterone from the Leydig cells of testes
- forms male internal sexual organs: Seminal vesicles, Epididymis, Ejaculatory duct, Ductus deferens
- needs to be induced to develop
- Paramesonephric (müllerian) duct
- default development but can be suppressed
- Female
- default phenotypic differentiation
- mesonephric duct degenerates and paramesonephric duct develops
- Male
- SRY gene (Y chromosome) produces testis-determining factor which is necessary for testes development
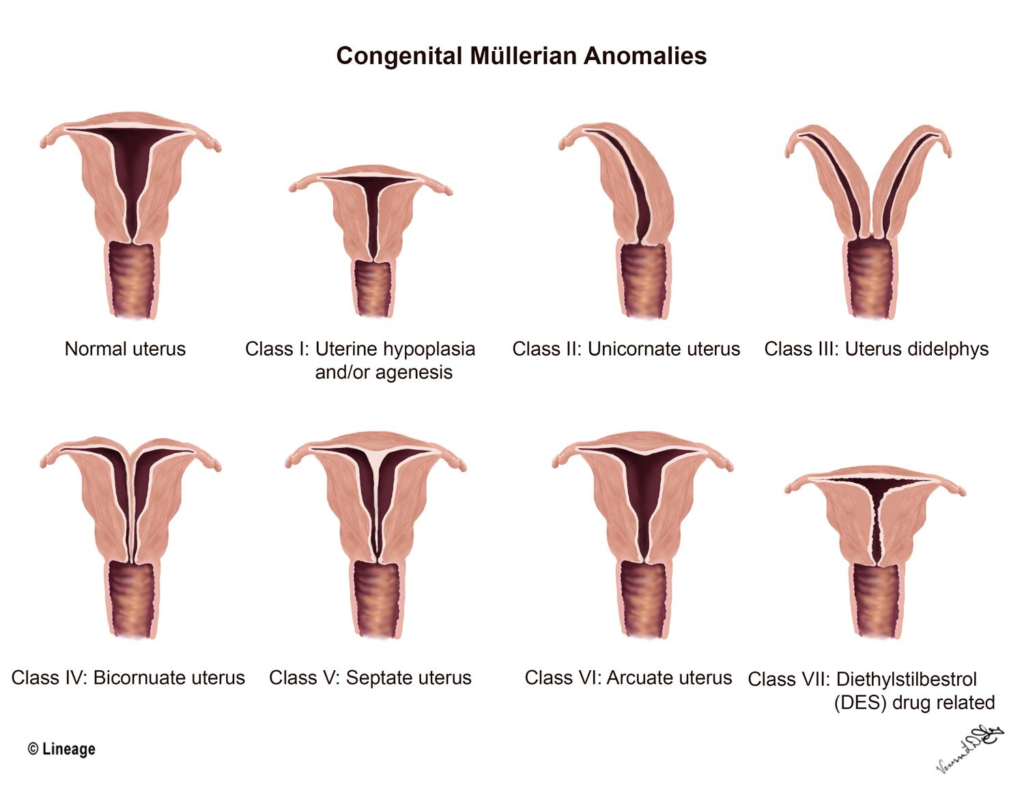
Female Genital Abnormalities
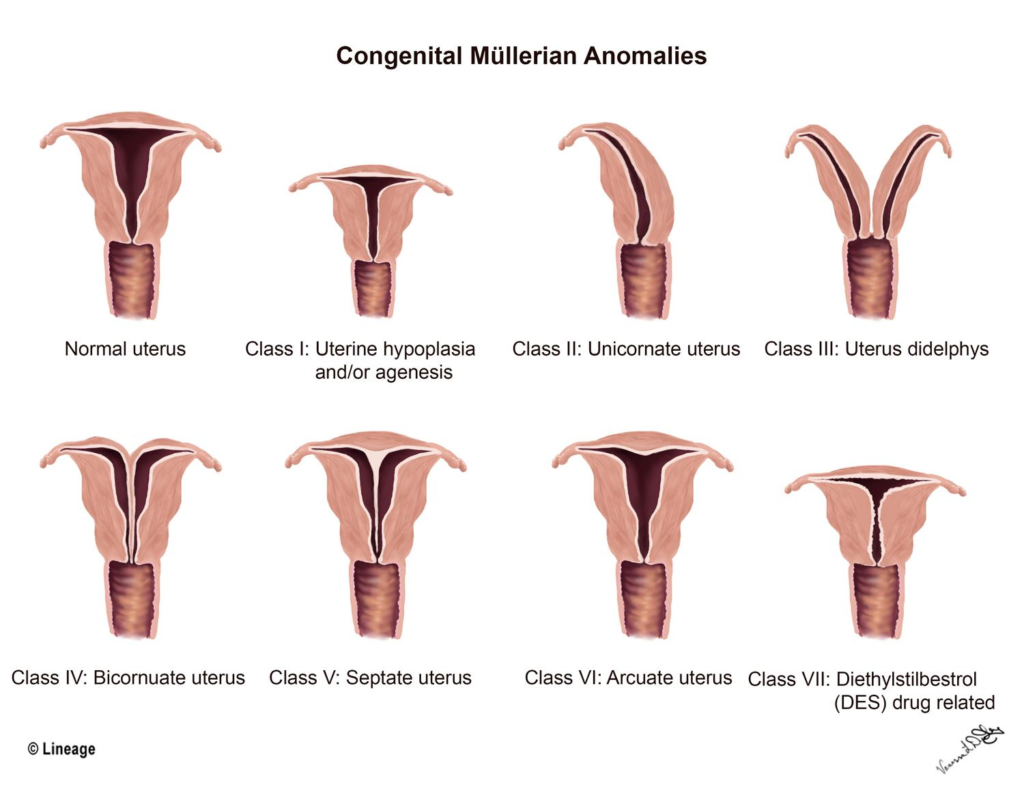
- Unicornate Uterus
- one paramesonephric fails to develop
- Bicornuate Uterus
- due to incomplete/partial fusion of the paramesonephric ducts
- associated with urinary tract abnormalities and infertility
- Uterus didelphys
- failure of paramesonephric ducts to develop resulting in abnormalities of the upper portion of the vagina, cervix, uterus, and fallopian tubes
Male Genital Abnormalities
- Hypospadias
- failure of urethral folds to fuse
- resulting in opening of penile urethra on inferior side of penis
- susceptible to UTI’s
- surgery is recommended for treatment
- Epispadias
- faulty positioning of genital tubercle
- resulting in penile urethra opening on superior side of penis
- associated with exstrophy of the bladder
- Cryptochidism
- failure of testes to descend into scrotum (undescended testes)
- testes can be found in inguinal canal or abdominal canal
- can lead to infertility if both are undescended
- observable within 3 months of birth
- Hydrocele
- processus vaginalis remains patent allowing fluid to flow in
- resulting in a fluid filled sac in the scrotum
- can differentiate from tumor by shining light through testes
- hydrocele allows light to flow through whereas a tumor does not


