Overview
Snapshot
- A 50-year-old man presents 4 months after an acute gout flare to his primary care physician. Since then, he has had 2 more episodes of minor flares that resolved on its own. He reports wanting better control of this disease. His physician describes several options for chronic gout and suggests allopurinol as a good first-line option.
Introduction
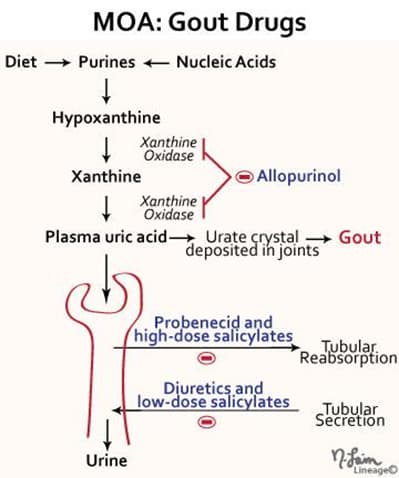
- Chronic gout drugs
- mechanism of action
- prevents the build up of uric acid
- drugs
- allopurinol
- febuxostat
- pegloticase
- probenecid
- mechanism of action
- Acute gout drugs
- mechanism of action
- reduces inflammation
- mechanism of action
- Drugs to avoid
- low-dose salicylates
- decreases uric acid excretion, which may precipitate gout
Allopurinol
- Mechanism of action
- Clinical use
- chronic gout
- prevention of urate nephropathy from tumor lysis syndrome in lymphoma and leukemia
- Toxicity
- ↑ accumulation of azathioprine and 6-mercaptopurine (MP)
- both are metabolized by xanthine oxidase
- ↑ accumulation of azathioprine and 6-mercaptopurine (MP)
- drug rash
Febuxostat
- Mechanism of action
- inhibition of xanthine oxidase
- Clinical use
- chronic gout
- Toxicity
- ↑ accumulation of azathioprine and 6-MP
- some hepatotoxicity
Pegloticase
- Mechanism of action
- pegloticase is a recombinant uricase
- catalyzes metabolism of uric acid to allantoin, which is more water-soluble
- pegloticase is a recombinant uricase
- Clinical use
- chronic gout
- Toxicity
- risk of new gout flare
- infusion reactions
Probenecid
- Mechanism of action
- inhibition of proximal convoluted tubule resorption of uric acid
- Clinical use
- chronic gout
- Toxicity
- uric acid calculi
- this should only be used in uric acid underexcreters and should be avoided in patients who are uric acid overproducers
- a history of prior uric acid stones is a contraindication for initiating this agent
- prolonged penicillin serum levels
- uric acid calculi
- inhibition of proximal convoluted tubule secretion of penicillin
Colchicine


