Snapshot
- A 25-year-old immigrant from Nigeria presents to the clinic with complaints of occasional fatigue. He has no other symptoms and denies any unexpected weight loss or night sweats. On exam, he has no lymphadenopathy. He does have mild splenomegaly and some conjunctival pallor. Labs reveal increased MCHC with intracellular crystals seen on blood smear.
Introduction
- Hemoglobinopathy with extravascular hemolysis
- hemoglobin C trait (HbAC) with no clinical symptoms
- hemoglobin C disease with mild hemolytic anemia and splenomegaly
- Hb C is a structural variant of normal hemoglobin (Hb A)
- Genetics
- autosomal recessive of β-Hb chain
- Pathogenesis
- Hb C is less soluble and crystalizes
- ↑ blood viscosity
- ↑ cellular rigidity
- shortened red cell survival
- Epidemiology
- common in Africa, southern Europe, South America, and Central America
- Potentially protects against malaria
- If co-inherited with Hb S (structural abnormality seen in sickle cell disease)
- Hb SC is less severe than Hb SS
- vaso-occlusive episodes
- vascular retinopathy
- avascular necrosis of femoral head
Presentation
- HbAC
- asymptomatic
- Hb C
- mild hemolytic anemia
- splenomegaly
- function is unaffected
- cholelithiasis with pigmented gallstones more common
Evaluation
- Diagnostic
- hemoglobin electrophoresis or high-performance liquid chromatography
- mostly Hb C
- absent Hb A
- ↑ Hb F (fetal Hb)
- hemoglobin electrophoresis or high-performance liquid chromatography
- ↑ MCHC may be noted
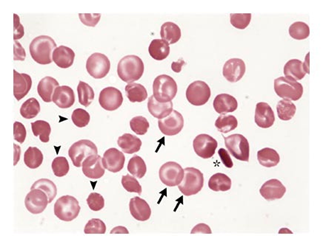
- Peripheral blood smear
- may show intracellular crystals
- may show target cells
- Markers of hemolysis
- ↑ LDH
- ↑ reticulocyte count
- ↑ indirect bilirubin
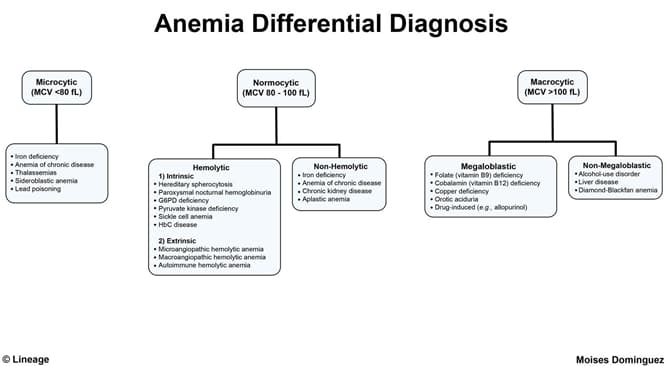
Differential Diagnosis
Treatment
- Supportive care
- folic acid supplementation
Prognosis, Prevention, and Complications
- Prognosis
- typically normal
- if co-inherited with hemoglobin S, life expectancy is in the 60s



