Snapshot – Hereditary Angioedema

- A 23-year-old woman with past medical history of multiple allergies leading to facial swelling presents with marked difficulty breathing, abdominal pain, and swelling of the face and neck. On physical exam, her extremities are also noted to be markedly swollen (picture). She is immediately sedated for intubation to maintain patency of airway. Chart review reveals newly-started ACE-inhibitor. She is given epinephrine, fluids, and fresh frozen plasma.
Introduction
- Disorder of complement, causing angioedema
- Genetics
- autosomal dominant
- Pathogenesis
- Epidemiology
- attacks begin during childhood
- Risk factors
- family history of angioedema
- family history of those contraindicated with ACE-inhibitors
- autoimmune conditions
Presentation
- Symptoms/physical exam
- recurrent episodes of angioedema without urticaria
- as opposed to anaphylaxis, which typically has urticarial
- angioedema of the face, oropharynx, extremities, or abdomen
- angioedema of GI tract
- severe abdominal pain
- GI upset
- worst at 24 hours
- resolves over 48-72 hours
- often preceded by prodrome
- fatigue
- flu-like symptoms
- recurrent episodes of angioedema without urticaria
- not responsive to epinephrine (epi-pen) or antihistamines
Evaluation
- Best initial test
- ↓ C4 and C2 levels
- if C4 are normal, C1 inhibitor deficiency is unlikely
- To confirm diagnosis if ↓ C4
- ↓ C1 inhibitor antigenic levels
- ↓ C1 inhibitor functional levels
Differential Diagnosis
- Anaphylaxis
- Allergic angioedema
- Facial cellulitis
- SVC syndrome
Treatment
- Anaphylaxis presents very similarly to angioedema and often cannot be differentiated immediately in an emergency room setting
- therefore, patients are often initially treated with medications for anaphylaxis given urgent, life-threatening nature of anaphylaxis
- epinephrine
- fluid replacement
- anti-histamines
- therefore, patients are often initially treated with medications for anaphylaxis given urgent, life-threatening nature of anaphylaxis
- Assess airway, even after administering treatment
- intubate if necessary
- As soon as possible, especially if epinephrine and anti-histamines are not effective, administer medications for hereditary angioedema
- plasma-derived C1 inhibitor
- recombinant human C1 inhibitor
- fresh frozen plasma if above are not available
Prognosis, Prevention, and Complications
- Prognosis
- mortaliy >30% in those with laryngeal angioedema
- angioedema is unpredictable
- Complications
- small bowel obstruction
- compartment syndrom
- death by asphyxiation
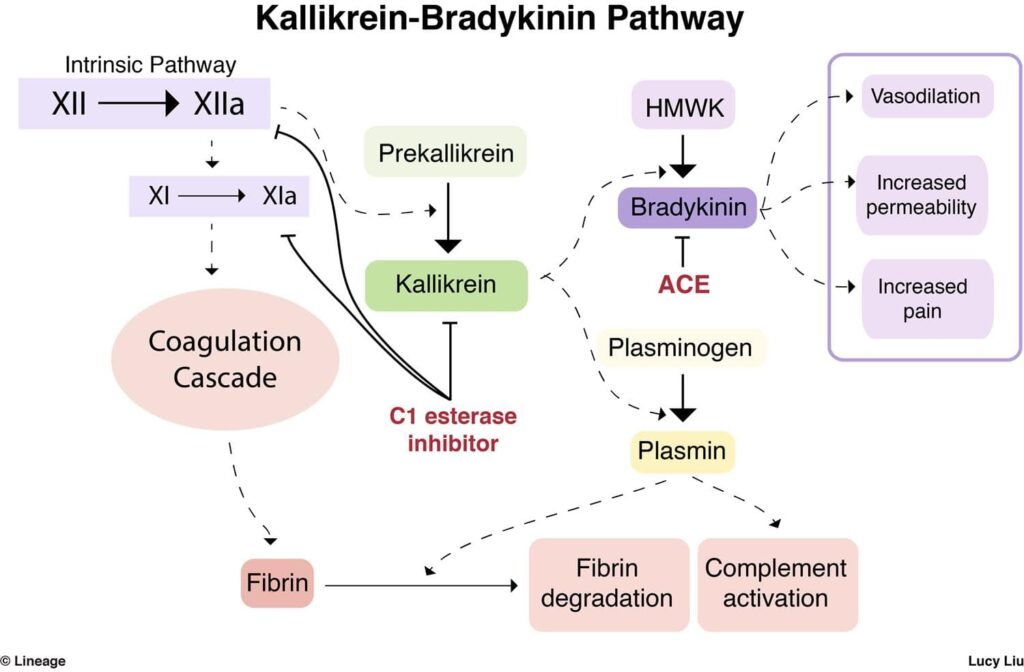
Hereditary Angioedema (HAE) is a rare genetic disorder characterized by recurrent episodes of severe swelling in various parts of the body. This condition is caused by a deficiency or dysfunction of C1 esterase inhibitor (C1-INH), a protein that regulates the complement and contact systems in the blood. Understanding Hereditary Angioedema is crucial for medical professionals, especially those in immunology, allergy, and emergency medicine. This article provides a comprehensive overview of Hereditary Angioedema, including its types, function, related studies, treatment considerations, and clinical significance.
Types of Hereditary Angioedema:
There are three main types of Hereditary Angioedema:
- Type I HAE: This type is characterized by a deficiency in the production of functional C1-INH protein.
- Type II HAE: Type II involves the production of dysfunctional C1-INH protein that does not effectively regulate complement and contact system activation.
- Type III HAE: This form is less common and primarily affects females. It is not associated with C1-INH deficiency but is often linked to mutations in the F12 gene, leading to increased production of bradykinin, a key mediator of angioedema.
Function of C1-INH:
C1-INH plays a crucial role in regulating two major blood pathways:
- Complement System: C1-INH controls the complement system, preventing excessive activation and the release of proinflammatory mediators.
- Contact System: C1-INH also regulates the contact system, which includes factors that, when activated, lead to the production of bradykinin—a potent vasodilator causing blood vessels to widen and become more permeable.
Clinical Manifestations:
Hereditary Angioedema is characterized by recurrent episodes of swelling that can affect various body parts, including:
- Skin: Swelling often occurs in the face, lips, tongue, and extremities.
- Gastrointestinal Tract: Swelling in the intestinal walls can cause severe abdominal pain, vomiting, and diarrhea.
- Respiratory Tract: In some cases, swelling of the airways can lead to life-threatening respiratory distress.
Hereditary Angioedema Studies:
- Genetic Studies: Research focuses on identifying mutations in the C1-INH gene or other genes associated with Type III HAE.
- Inflammatory Pathways: Studies investigate the molecular pathways involved in bradykinin production and its role in angioedema.
Clinical Significance:
- Risk of Anaphylaxis: Severe angioedema episodes, especially those involving the respiratory tract, can lead to anaphylactic shock, which can be fatal.
- Quality of Life Impact: The recurrent nature of HAE and its unpredictable attacks can significantly impact a patient’s quality of life.
Future Directions:
- Targeted Therapies: Research explores targeted therapies that can specifically inhibit bradykinin production or its effects.
- Gene Therapy: Advances in gene therapy may offer potential treatments, particularly for Type III HAE.
Conclusion:
Hereditary Angioedema is a rare genetic disorder characterized by recurrent episodes of severe swelling in various parts of the body. It results from a deficiency or dysfunction of C1-INH, a protein that regulates the complement and contact systems in the blood. HAE can significantly impact a patient’s quality of life and carries the risk of life-threatening anaphylactic reactions. Research in genetics and inflammatory pathways enhances our understanding of this condition, leading to improved treatment strategies.
Check out USMLE Success Strategy: Personalized Consultation and Study Plan Development.


