Snapshot – Hyper IgM Syndrome
- A 6-month-old boy presents with a past medical history of skin infections presents with difficulty breathing, high fever, and nonproductive cough. He is immediately started on broad-spectrum antibiotics. On further questioning, his family history includes a maternal uncle dying at age 20 from overwhelming pneumonia. Sputum is induced with hypertonic saline inhalation, and eventual staining shows Pneumocystis. He is immediately started on IVIG.
Introduction
- Inherited primary combined B- and T-cell immunodeficiency characterized by increased levels of IgM
- Genetics
- X-linked recessive
- mutation in gene that codes for CD40 ligand (CD40L)
- Pathogenesis
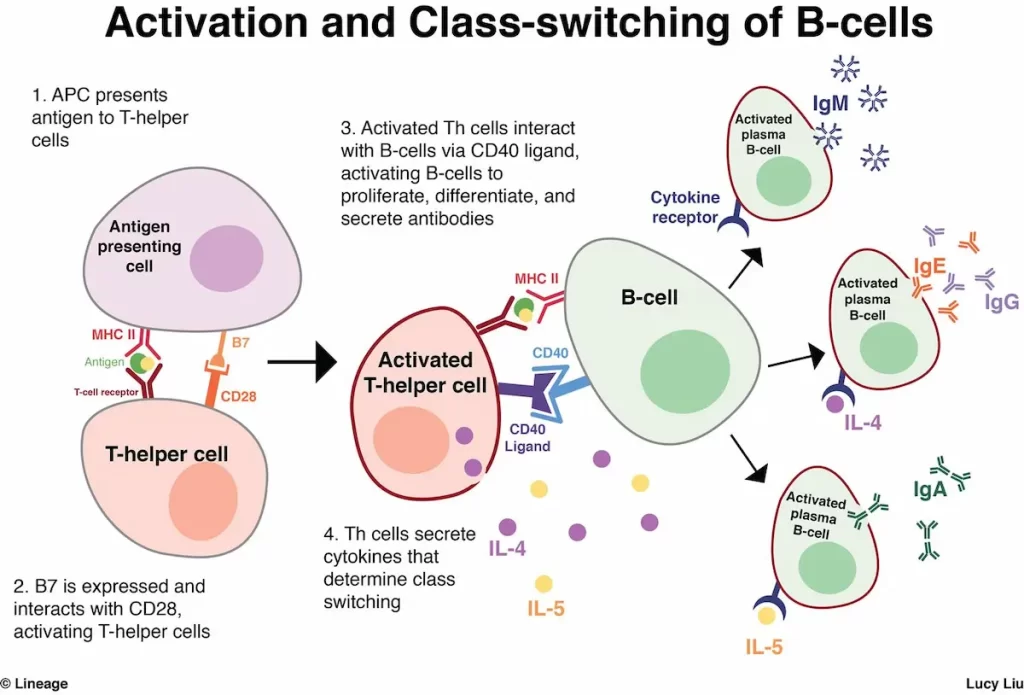
- CD40L is expressed on activated T-helper cells
- defect in humoral immunity
- defect cell-mediated immunity
- CD40L also required for maturation of T-cells, dendritic cells, and macrophages
- Symptoms onset by 1 year, often with Pneumocystis infections
- most diagnosed before 4 years
Presentation
- Symptoms
- severe pyogenic infections early in life
- chronic diarrhea
- opportunistic infections
- pneumonia
- Pneumocystis
- Cryptosporidium
- CMV
- echovirus encephalitis
- pancytopenia common
- fatigue
- infection
- pallor
- bleeding
Evaluation
- Ig levels
- Diagnosis confirmed with flow cytometry
- deficient expression of CD40L on activated T-helper cells
- normal T- and B-cells
- CBC
- neutropenia
- thrombocytopenia possible
Differential Diagnosis
Treatment
- Prophylaxis of Pneumocystis
- Regular IVIG replacement
Prognosis, Prevention, and Complications
- Prognosis
- 20% survival rate past young adulthood
- leading cause of death
- pneumonia
- encephalitis
- malignancy
- Complications
- increased risk of autoimmunity
- increased risk of malignancies
- HCC
- carcinoid tumor
- infection
- bronchiectasis
Hyper IgM Syndrome is a rare primary immunodeficiency disorder characterized by elevated levels of immunoglobulin M (IgM) antibodies and reduced levels of other immunoglobulins, particularly IgG and IgA. This condition results from genetic mutations that affect the ability of B cells to switch from producing IgM to other antibody classes. Understanding Hyper IgM Syndrome is crucial for medical professionals, especially those in immunology, pediatrics, and infectious diseases. This article provides a comprehensive overview of Hyper IgM Syndrome, including its types, function, related studies, treatment considerations, and clinical significance.
Types of Hyper IgM Syndrome:
There are several types of Hyper IgM Syndrome, each associated with different genetic mutations:
- X-Linked Hyper IgM Syndrome (XHIGM): This is the most common form and results from mutations in the CD40 ligand (CD40L) gene located on the X chromosome.
- Autosomal Recessive Hyper IgM Syndrome (AR-HIGM): This form is caused by mutations in other genes, including AID (activation-induced cytidine deaminase) and UNG (uracil-DNA glycosylase), which are involved in the antibody class-switching process.
Function and Genetic Basis:
Hyper IgM Syndrome is primarily caused by mutations in genes that play crucial roles in the antibody class-switching process. These mutations lead to the inability of B cells to switch from producing IgM to other antibody classes like IgG, IgA, and IgE.
Clinical Manifestations:
Hyper IgM Syndrome presents with a range of clinical features:
- Recurrent Infections: Reduced levels of IgG and IgA antibodies compromise the ability to mount effective immune responses against bacterial, viral, and fungal infections.
- Opportunistic Infections: Patients are particularly susceptible to opportunistic infections, including Pneumocystis jirovecii pneumonia (PCP) and Cryptosporidium.
- Autoimmunity: Some individuals with Hyper IgM Syndrome develop autoimmune conditions due to dysregulated immune responses.
Hyper IgM Syndrome Studies:
- Genetic Studies: Research focuses on identifying genetic mutations responsible for different types of Hyper IgM Syndrome.
- B-Cell Biology: Studies investigate the underlying mechanisms that lead to the impairment of antibody class-switching in B cells.
Clinical Significance:
- Immunodeficiency: Hyper IgM Syndrome leads to significant immunodeficiency, resulting in recurrent and severe infections.
- Opportunistic Infections: The susceptibility to opportunistic infections can have serious consequences for patients.
Treatment Considerations:
- Infection Management: Treatment involves aggressive management of infections with appropriate antimicrobial agents.
- Immunoglobulin Replacement: Regular infusions of immunoglobulins, particularly IgG, help provide passive immunity and reduce infection risk.
- Stem Cell Transplantation: In severe cases, hematopoietic stem cell transplantation may be considered to replace the defective immune system.
Future Directions:
- Gene Therapy: Research explores the potential of gene therapy to correct genetic mutations causing Hyper IgM Syndrome.
- Immunomodulation: Investigative therapies aim to modulate immune responses and improve antibody class-switching.
Conclusion:
Hyper IgM Syndrome is a rare primary immunodeficiency disorder characterized by elevated IgM levels and reduced levels of other immunoglobulins. Genetic mutations disrupt the antibody class-switching process, leading to impaired immune responses against infections and increased susceptibility to opportunistic infections. The syndrome is associated with various clinical manifestations, including recurrent infections and autoimmunity. Genetic studies aim to identify mutations, while research in B-cell biology explores the mechanisms underlying antibody class-switching.
Check out Ultimate USMLE Step 1 Study Notes.


