Snapshot
- A 59-year-old woman presents to the emergency room with severe low back pain. She reports pain radiating down her left leg into her left foot. The pain started after lifting multiple heavy boxes at her work as a grocery store clerk. On exam, she is unable to bend over due to pain. A straight leg raise elicits severe radiating pain into her left lower extremity. The patient reports that the pain is worst along the posterior thigh and posterolateral leg into the fourth and fifth toes.
Introduction
- Clinical definition
- a condition in which the central portion of the intervertebral disc herniates beyond the firm outer ring
- can lead to spinal inflammation +/- nerve root compression
- also known as a slipped disc, herniated disc, or herniated nucleus pulposus (HNP)
- a condition in which the central portion of the intervertebral disc herniates beyond the firm outer ring
- Epidemiology
- demographics
- male:female ratio is approximately 2:1
- peak incidence in 4th and 5th decades
- location
- lumbar >> cervical > thoracic
- risk factors
- manual labor
- heavy lifting
- competitive sports
- demographics
- Pathophysiology
- normal anatomy
- intervertebral disc
- functions
- permit spinal motion
- link adjacent vertebral bodies
- provide 25% of spinal column height
- composition
- annulus fibrosis
- thick outer layer of disc
- composed of type I collagen, water, and proteoglycans
- nucleus pulposus
- soft central layer of disc
- composed of type II collagen, water, and proteoglycans
- annulus fibrosis
- functions
- intervertebral disc
- pathoanatomy
- torsional strain leads to degeneration and tears in the annulus fibrosis
- nucleus pulposus is able to protrude through the torn annulus fibrosis
- leads to release of inflammatory markers and may compress a nearby nerve root
- nucleus pulposus can herniate in different directions (e.g., posterolaterally, laterally, and centrally)
- direction of herniation (e.g., posterolateral vs. far lateral) and the location of the herniation within the spine (e.g., lumbar vs. cervical) may change the nerve root that is compressed
- normal anatomy
- Associated conditions
- cauda equina syndrome
- rare
- caused by a large disc herniation compressing the nerve roots at the end of the spinal cord
- radicular pain
- may occur if descending nerve roots into lower extremity are compressed
- cauda equina syndrome
- Prognosis
- natural history of disease
- 90% of patients will experience symptom improvement within 3 months with nonoperative management
Presentation
- Lumbar disc herniation
- symptoms
- low back pain
- radicular leg pain
- radiates from the buttock into the leg
- worsens with sitting, coughing, valsalva, and sneezing
- improves with standing
- physical exam
- motor exam
- provocative tests
- straight leg raise
- elicit pain and paresthesias in the leg at 30-70 degrees of hip flexion
- caused by tension in the L5 or S1 nerve roots
- bowstring sign
- straight leg raise that is aggravated by compression of the popliteal fossa
- straight leg raise
- symptoms
- Cervical disc herniation
- symptoms
- occipital headache
- neck pain
- unilateral arm pain, numbness, weakness, and/or tingling
- physical exam
- motor exam
- provocative tests
- Spurling test
- test by extending head, rotating and laterally bending to the affected side, and vertically compressing the head downward
- Spurling test
- symptoms
- positive if this maneuver reproduces pain in the ipsilateral arm
Imaging
- Radiographs
- indications
- radiographs not typically indicated
- findings
- often normal
- may demonstrate loss of disc height or loss of lordosis
- indications
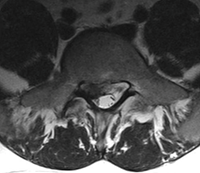
- MRI
- indications
- not typically indicated unless operative management is being considered
- indications
- best imaging modality to characterize site and extent of lesion
Differential
- Paraspinal muscle strain
- distinguishing factors
- will not present with radicular pain
- will typically resolve within 6 weeks
- distinguishing factors
- Spondylolisthesis
- distinguishing factors
- radiographs will demonstrate slippage of one vertebrae relative to the inferior vertebrae
Treatment
- Nonoperative
- rest, physical therapy, and anti-inflammatory medications
- indications
- first-line treatment for the majority of patients with intervertebral disc herniations
- indications
- nerve root corticosteroid injections
- indications
- alternative treatment if physical therapy and medications fail
- indications
- rest, physical therapy, and anti-inflammatory medications
- Operative
- microdiscectomy
- indications
- failure of nonoperative management
- indications
- microdiscectomy
- cauda equina syndrome
Complications
- Cauda equina syndrome
- incidence
- occurs in 1-10% of lumbar disc herniations
- incidence


