Snapshot – Leukocyte Adhesion Deficiency
- A 4-day-old girl born to a G1P1 mother with no complications presents with a fever. There is some swelling with serosanguinous fluids around her rectum. Cultures from the fluid grow Staphylococcus spp and is treated with antibiotics. On day 15 of life, she develops an ear infection and is once again treated with antibiotics. The umbilical cord is still attached, and on day 34 of life, the umbilical stump is noted to be erythematous, indurated, and tense. A completel blood cell count is significant for leukocytosis. Immunoglobulin levels are normal. Flow cytometry reveals decreased expression of CD18 to < 1%.
Introduction
- Primary immunodeficiency resulting from phagocytic dysfunction
- Genetics
- autosomal recessive
- absence or defective CD18
- Epidemiology
- very rare
- primarily seen in pediatric population
- Pathogenesis
- defect in LFA-1 integrin (CD18) protein on leukocytes
- normal physiology
- CD11a/CD18 (LFA-1 integrin) expressed on lymphocytes are important in the
- trafficking and adhesion to vascular endothelium
- interactions with antigen presenting cells
- cytotoxic T-cell killing
- CD11a/CD18 (LFA-1 integrin) expressed on lymphocytes are important in the
- results in impaired migration and chemotaxis
- Prognosis
- 75% of individuals have severe disease, with typically < 1% expression of CD18
- may succumb to life-threatening infection within 1-2 years of life
- mild disease, with 1-30% expression of CD18
- 75% of individuals have severe disease, with typically < 1% expression of CD18
- survive to adulthood
Presentation
- Symptoms
- delayed separation of umbilical cord at birth to > 30 days
- omphalitis
- recurrent infections of skin and mucosa
- most commonly due to Staphylococcus spp., enteric gram-negative bacteria, and fungi
- perirectal and labial cellulitis
- otitis media
- absent pus formation
- serosanguineous fluids may be present
- impaired wound healing
- poorly formed, thin, bluish scars
- gingivostomatitis
Evaluation
- ↑ Neutrophils in the absence of infection
- dramatically ↑ with infection
- Histology
- localized infection with absence of neutrophils or pus
- edema and necrosis
- Flow cytometry
- absence of CD18 on leukocytes
Differential Diagnosis
Treatment
- Hematopoietic stem cell transplant
- high success rate
- Prophylactic antibiotics
Complications
- Life-threatening infections
- Graft versus host disease after stem cell transplant
Leukocyte Adhesion Deficiency Type I (LAD-I) is a rare genetic disorder that affects the immune system, specifically impairing the ability of white blood cells (leukocytes) to adhere to and migrate through blood vessel walls to sites of infection or injury. This condition leads to recurrent and severe bacterial infections, delayed wound healing, and other health complications. Understanding LAD-I is crucial for medical professionals, particularly those in immunology, pediatrics, and infectious diseases. This article provides a comprehensive overview of Leukocyte Adhesion Deficiency Type I, including its types, function, related studies, treatment considerations, and clinical significance.
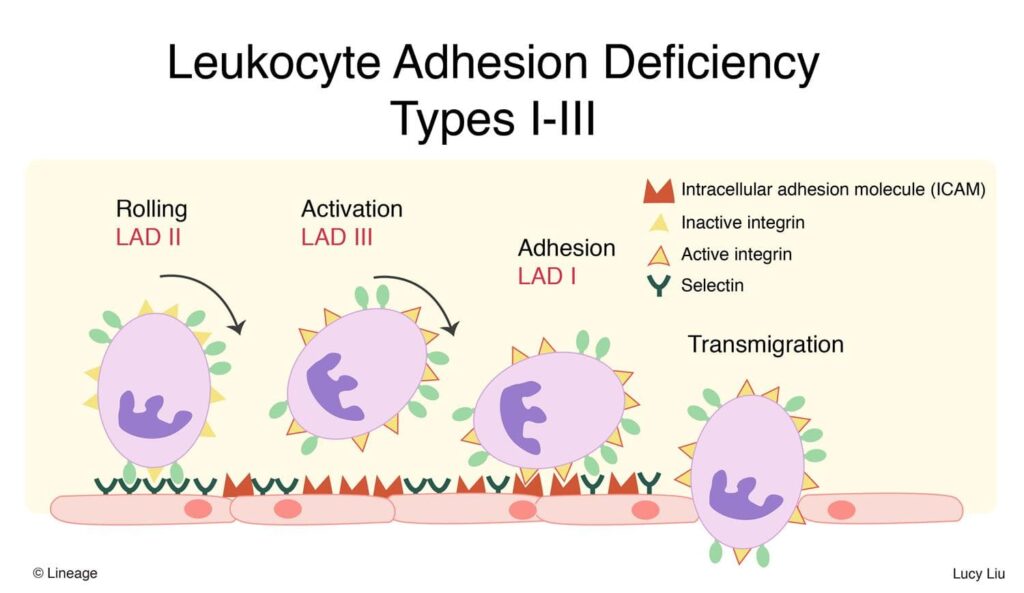
Types of Leukocyte Adhesion Deficiency:
There are three known types of Leukocyte Adhesion Deficiency, with LAD-I being the most common and well-understood:
- LAD-I (CD18 Deficiency): This form results from mutations in the ITGB2 gene, which encodes the CD18 protein component of the β2 integrin family.
- LAD-II (Sialyl-Lewis X Deficiency): LAD-II is extremely rare and caused by mutations in the SLC35C1 gene. It affects glycosylation processes, impacting the selectin-mediated adhesion of leukocytes to endothelial cells.
- LAD-III (Kindlin-3 Deficiency): LAD-III is also rare and results from mutations in the FERMT3 gene, affecting integrin activation and leukocyte adhesion.
Function of Leukocyte Adhesion:
Leukocyte adhesion is a critical step in the immune response, allowing white blood cells to:
- Migrate to Infection Sites: Leukocytes need to attach to and pass through the blood vessel walls to reach sites of infection or injury in the tissues.
- Phagocytosis: Once at the site of infection, leukocytes must adhere to pathogens and engulf them through a process called phagocytosis.
Clinical Manifestations:
Leukocyte Adhesion Deficiency-I presents with a range of clinical features:
- Recurrent Infections: Patients with LAD-I experience frequent and severe bacterial infections affecting the skin, respiratory system, and gastrointestinal tract.
- Delayed Wound Healing: Impaired leukocyte function leads to slow wound healing and the formation of chronic, non-healing ulcers.
- Gingivitis and Periodontal Disease: Oral symptoms such as gingivitis, periodontal disease, and dental abscesses are common due to poor leukocyte response to oral bacteria.
LAD-I Studies:
- Genetic Studies: Research focuses on identifying mutations in the ITGB2 gene and their impact on CD18 protein function.
- Leukocyte Adhesion Mechanisms: Studies investigate the molecular mechanisms involved in leukocyte adhesion and migration.
Clinical Significance:
- Risk of Infections: Leukocyte Adhesion Deficiency-I patients are highly susceptible to recurrent bacterial infections, some of which can be life-threatening.
- Chronic Inflammation: The inability to resolve infections can lead to chronic inflammation and tissue damage.
Future Directions:
- Gene Editing: Advances in gene editing techniques like CRISPR-Cas9 hold promise for correcting genetic mutations in Leukocyte Adhesion Deficiency-I.
- Immunomodulatory Therapies: Research aims to develop therapies that can improve leukocyte function in LAD-I patients.
Conclusion:
Leukocyte Adhesion Deficiency Type I is a rare genetic disorder that impairs the ability of white blood cells to adhere to and migrate through blood vessel walls to sites of infection or injury. This condition results from mutations in the ITGB2 gene, leading to recurrent and severe bacterial infections, delayed wound healing, and other complications. Research focuses on identifying genetic mutations and understanding the mechanisms of leukocyte adhesion. Treatment options include antibiotic prophylaxis, stem cell transplantation, and experimental gene therapies. Advances in gene editing and immunomodulatory therapies hold promise for improving the lives of individuals with LAD-I.
Check out Interview Preparation, CV and Personal Statement Editing – The Finale.


