Introduction
- Epidemiology
- breast cancer is the most common cancer and second most common cause of death in adult women
- Risk factors
- BRCA1 and BRCA2 mutations
- associated with multiple / early onset breast and ovarian cancer
- other genetic relationships
- RAS oncogene gain of function
- overexpression of estrogen/progesterone receptors
- overexpression of erb-B2 (HER-2, an EGF receptor)
- Li-Fraumeni associated TP53 loss
- increasing age
- smoking
- breast cancer in first degree relatives or mother with breast cancer
- history of contralateral breast cancer
- history of endometrial cancer
- also an estrogen induced cancer
- increased exposure to estrogen
- obesity
- nulliparity
- early menarche (<11 y.o.)
- late menopause (>50 y.o.)
- late first pregnancy (>30 y.o.)
- BRCA1 and BRCA2 mutations
- atypical ductal hyperplasia
Classification
- Ductal carcinoma in situ (DCIS)
- arises from progression of ductal hyperplasia
- non-palpable mass
- seen most often on mammography due to microcalcifications
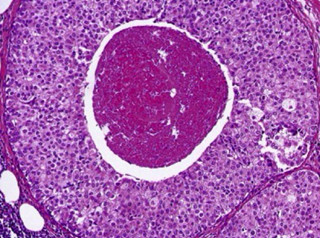
- histology shows filled ductal lumen without basement membrane penetration
- Paget’s disease
- Invasive/infiltrating ductal carcinoma
- worst and most invasive
- most common type
- firm, fibrous, “rock-hard” mass
- histology shows small, glandular, duct-like cells with stellate morphology
- subtypes
- tubular carcinoma
- histology
- well-differentiated tubules that lack myoepithelial cells
- histology
- mucinous carcinoma
- histology
- carcinoma with abundant extracellular mucin
- histology
- tubular carcinoma
- Lobular carcinoma in situ (LCIS)
- non-palpable mass
- often bilateral
- Invasive lobular
- often multiple and bilateral
- Medullary
- associated with BRCA1 and ER/PR negativity
- histology shows fleshy, cellular, lymphatic infiltrate
- Inflammatory
- poor prognosis (50% survival at 5 years)
- histology shows dermal lymphatic invasion by tumor
- see below
Presentation
- Symptoms
- often asymptomatic
- breast lump
- most commonly in upper-outer quadrant
- nipple discharge
- Physical exam
- firm immobile, painless lump
- some skin changes
- redness, ulcerations, edema, and nodularity
- axillary lymphadenopathy
- in more advanced cases
- breast skin edema with dimpling (peau d’ orange)
- represents obstruction of the lymphatics by cancer
Evaluation
- Fine needle aspiration
- can identify whether mass is solid or cystic
- can also retrieve sample for cancer diagnosis
- Estrogen/Progesterone receptor assays
- most often positive in post-menopausal cancers
- low estrogen state after menopause results in upregulation of receptors
- positivity confers better prognosis with more effective therapeutics
- most often positive in post-menopausal cancers
- Sentinel lymph node biopsy
- if negative high likelihood no other nodes in group are involved
- if positive there is 1/3 chance other nodes in group are involved
Treatment
- Surgery
- breast conservation resection
- resection of tumor with margins
- sentinel node biopsy
- radiation
- breast conservation resection
- lymphedema
Prognosis, Prevention, and Complications
- Prognosis
- lymph node involvement is the single most important prognostic factor
- TNM staging
- extranodal metastases has more significance than lymph node metastasis
- Prevention
- mammography
- effective screening tool except in young woman
- dense breast tissue in young woman interferes with specificity and sensitivity
- most effective in postmenopausal patients because of less glandular breast
- identifies microcalcifications or moderate sized masses
- all woman > 40 should have mammograms
- effective screening tool except in young woman
- mammography



