Introduction
- Pathophysiology
- aka hyaline membrane disease
- reduced surfactant results in low lung compliance and subsequent atelectasis, intrapulmonary shunting, and acute lung injury
- Causes
- prematurity (most important)
- increased fetal blood glucose results in increased fetal insulin production
Presentation
- Symptoms
- dyspnea, tachypnea during first hours of life
- nasal flaring
- expiratory grunting,
- intercostal, subxiphoid retractions
- Physical exam
- severe hypoxemia
- not responsive to 100% O2
- atelectasis results in intrapulmonary (right-to-left) shunting
- not responsive to 100% O2
- severe hypoxemia
- perfusion without ventilation
Evaluation
- ABG
- hypoxemia
- Histology
- hyaline membrane surrounds collapsed alveoli
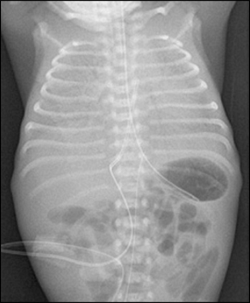
- CXR
- Amniotic fluid
- lecithin:sphingomyelin ratio < 1.5
Treatment
Complications
- Bronchopulmonary dysplasia
- still very common
- Patent ductus arteriosus
- normally closed by increased O2 tension at birth
- hypoxia keeps shunt open
- normally closed by increased O2 tension at birth
- 100% O2 therapy damage
- damage also when the neonate is taken off oxygen therapy
- upregulation of VEGF due to relative hypoxia results in neovascularization in the retina (retinopathy of prematurity)
- damage also when the neonate is taken off oxygen therapy


