Overview
Snapshot
- A 68-year-old woman presents to her primary care physician with lower back pain of acute onset. She denies any trauma to the spine or any radiation of pain. Her last menstrual period was when she was 51-years-old. On physical exam, she has tenderness to palpation at the level of L4-L5, as well as a loss of lumbar lordosis. A dual-energy x-ray absorptiometry (DEXA) scan reveals a T-score of -2.7.
Introduction
- Clinical definition
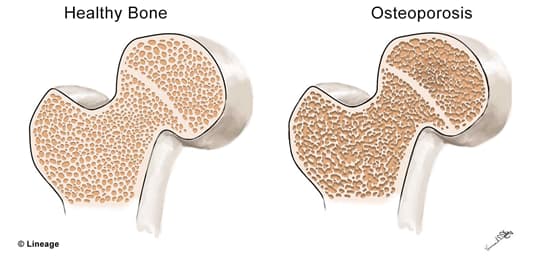
- decreased bone mass (osteopenia) that significantly increases the patient’s risk of fracture
- Epidemiology
- incidence
- most common types of osteoporosis are
- post-menopausal
- senile
- most common types of osteoporosis are
- risk factors
- post-menopausal women
- being ≥ 65 years of age
- people of Caucasian and Asian descent
- lifestyle factors
- poor physical activity
- vitamin D deficiency and poor calcium intake
- smoking
- alcohol use disorder
- hyperparathyroidism
- hyperthyroidism
- multiple myeloma
- malabsorption syndromes
- low body weight
- higher body weight associated with higher bone density
- incidence
- Pathogenesis
- in young adulthood, peak bone mass is achieved and this is determined by a number of factors (e.g., genetics)
- after this peak bone mass is attained, there is a small decrease in bone formation with every cycle of bone remodeling
- senile osteoporosis
- osteoblasts have their biosynthetic and proliferative ability reduced with age
- poor physical activity
- mechanical force on bone stimulates bone remodeling
- athletes have increased bone density
- decreased physical activity results in bone loss
- mechanical force on bone stimulates bone remodeling
- decreased estrogen levels
- such as in menopause, decreased estrogen levels increase bone resportion and formation
- however, the rate of formation is less than resorption resulting in a net bone loss
- such as in menopause, decreased estrogen levels increase bone resportion and formation
- senile osteoporosis
- after this peak bone mass is attained, there is a small decrease in bone formation with every cycle of bone remodeling
- in young adulthood, peak bone mass is achieved and this is determined by a number of factors (e.g., genetics)
- Prognosis
- generally good if detected early and appropriately managed
Presentation
- Symptoms
- fractures (e.g., vertberal and hip), otherwise, patients are typically asymptomatic
- Physical exam
- may see loss in height
Imaging
- DEXA
- indication
- all women ≥ 65 and all men ≥ 70 years of age
- notes
- indication
- T-score ≤ -2.5
Studies
- Labs
- Histology
- histologically normal; however, there is a decreased quantity of normal bone
Differential
Treatment
- Conservative
- calcium and vitamin D supplementation
- strength training
- smoking cessation
- Medical
- bisphosphonates
- indication
- first-line for pharmacologic therapy in osteoporosis
- indication
- teriparatide
- indication
- bisphosphonates
- considered first-line in patients with a very high risk of fracture
Complications
- Fragility fractures
- hip
- distal radius
- vertebral body
- proximal humerus


