Hypoxemia
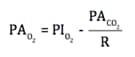
- Alveolar gas equation
- predicts the change in PAO2 that will occur for a given change in PACO2
- PAO2 = alveolar PO2
- PIO2 = PO2 in inspired air
- normally, PIO2 = 150 mm Hg
- PACO2 = alveolar PCO2
- R = respiratory exchange ratio = (CO2 production) / (O2 consumption)
- normally, R = 0.80
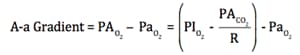
- A-a Gradient
- alveolar PO2 (PAO2) – systemic arterial PO2 (PaO2)
- normal A-a gradient = 15 mm Hg (~Age/4 +4)
- equilibration of O2 across alveolar gas and pulmonary capillary blood
- pulmonary capillary blood becomes systemic arterial blood
- increases with age
- equilibration of O2 across alveolar gas and pulmonary capillary blood
- hypoxemia → ↑ A-a gradient
- e.g., shunt, V/Q mismatch, pulmonary fibrosis (diffusion defect)
- Causes of Hypoxemia (↓ PaO2)
- High Altitude (normal A-a gradient)
- a decrease in barometric pressure (PB) decreases the PIO2 of inspired air
- FiO2 doesn’t change (21%)
- ↓ PB → ↓ PIO2 → ↓ PAO2 → ↓ PaO2
- a decrease in barometric pressure (PB) decreases the PIO2 of inspired air
- Hypoventilation (normal A-a gradient)
- a decrease in minute ventilation (respiratory rate x tidal volume) decreases PAO2
- ↓ ventilation → ↑ PACO2 → ↓ PAO2
- FiO2 and PB don’t change in alveolar gas equation
- a decrease in minute ventilation (respiratory rate x tidal volume) decreases PAO2
- V/Q Mismatch (↑ A-a gradient)
- Diffusion Limitation (↑ A-a gradient)
- e.g., pulmonary fibrosis
- ↑ diffusion distance for diffusion
- e.g., pulmonary edema
- ↓ surface area for diffusion, ↑ diffusion distance
- e.g., pulmonary fibrosis
- Right-to-Left Shunt (↑ A-a gradient)
- High Altitude (normal A-a gradient)
- low O2 shunted blood mixes with and dilutes high O2 non-shunted blood
Hypoxia
- Decreased Oxygen Delivery to Tissues
- O2 content of blood = (O2 binding capacity) x (% saturation) + dissolved O2
- (O2 binding capacity) x (% saturation) = O2 bound to hemoglobin
- O2 delivery = (cardiac output) x (O2 content of blood)
- O2 content of blood = (O2 binding capacity) x (% saturation) + dissolved O2
- Causes of Hypoxia (↓ O2 Delivery to Tissues)
- circulatory (↓ Cardiac Output)
- ↓ blood flow
- anemic (see CO poisoning below)
- ↓ concentration of hemoglobin→ ↓ O2 content of blood
- histotoxic (example: cyanide poisoning)
- ↓ O2 utilization by tissues (mitochondrial poison)
- circulatory (↓ Cardiac Output)
- not common in living patients
Ischemia
- Causes of Ischemia (↓ Blood Flow)
- ↓ arterial blood flow
- e.g., atherosclerosis
- ↓ venous return
- e.g., Budd-Chiari syndrome
- ↓ arterial blood flow


