Overview
- Overview
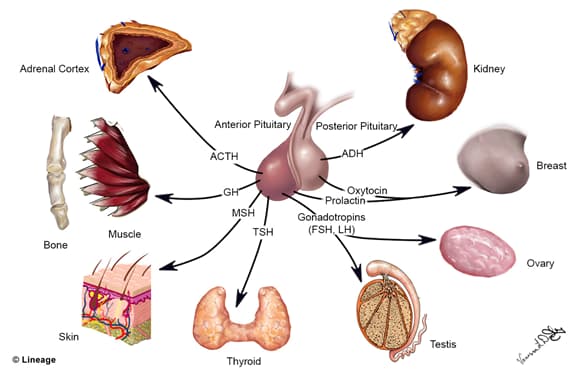
- pituitary, or hypophysis, rests in sella turcica, a depression of the sphenoid bone
- primary function of pituitary is secretion of hormones
- anatomically, pituitary is divided into anterior and posterior pituitary
Anterior Pituitary: Anatomy and Embryology
- Anterior pituitary
- anterior pituitary, or adenohypophysis, is the glandular component of the pituitary
- a collection of endocrine cells
- responsible for synthesis and secretion of anterior pituitary hormones
- a collection of endocrine cells
- consists of pars distalis, pars intermedia,and pars tuberalis
- anterior pituitary, or adenohypophysis, is the glandular component of the pituitary
- Anterior pituitary cell types
- various cell types are responsible for synthesis and secretion of various hormones
- gonadotrophs
- FSH and LH
- corticotrophs
- ACTH
- thyrotrophs
- TSH
- lactotrophs
- prolactin
- somatotrophs
- growth hormone (somatotropin)
- Histology
- chromophils
- anterior pituitary cells that contain granules that react with acidophilic/basophilic stains
- acidophils
- anterior pituitary cells (pars distalis) that contain granules that react with acidophilic stains
- responsible for synthesis and secretion of PiG hormones
- prolactin and growth hormone
- acidophils
- anterior pituitary cells that contain granules that react with acidophilic/basophilic stains
- chromophobes
- anterior pituitary cells that lack granules and that do not react with acidophilic/basophilic stains
- chromophils
- e.g., stromal cells and degranulated chromophils
Anterior Pituitary: Hormones
- Anterior pituitary hormones
- FLAT PiG
- FSH (follicle-stimulating hormone)
- LH (luteinizing hormone)
- ACTH (adrenocorticotropic hormone)
- Prolactin
- Growth hormone (somatotropin)
- categories of hormones
- corticolipotropins
- ACTH and MSH (melanocyte-stimulating hormone)
- glycoprotein hormones
- FSH, LH, TSH
- somatomammotropins
- prolactin and growth hormone
- corticolipotropins
- FLAT PiG
- Cortiolipotropins
- Glycoprotein hormones
- subunits of peptide hormones
- glycoprotein hormones contain 2 subunits: α and β subunit
- α subunits identical, β subunits non-identical
- hormone specificity determined by β subunit
- α subunits identical, β subunits non-identical
- human chorionic gonadotropin (hCG) structurally related to glycoprotein hormone
- hCG contains identical α subunit
- glycoprotein hormones contain 2 subunits: α and β subunit
- subunits of peptide hormones
- Somatomammotropins
- growth hormone
- secretion
- pulsatile secretory pattern
- secretory bursts approximately every 2 hours
- ↑ in secretory bursts during exercise and sleep
- secretory bursts approximately every 2 hours
- pulsatile secretory pattern
- functions
- ↑ linear growth and muscle mass
- growth mediated by production of somatomedins
- aka insulin-like growth factors (IGFs)
- growth mediated by production of somatomedins
- diabetogenic effect
- insulin resistance
- decreases glucose uptake and utilization
- “diabetogenic”
- growth hormone produces increases in blood glucose
- insulin resistance
- ↑ linear growth and muscle mass
- pathophysiology
- GH deficiency
- before puberty
- symptoms
- failure to grow
- short stature
- mild obesity
- delayed puberty
- symptoms
- treatment
- growth hormone replacement
- before puberty
- GH excess
- growth-hormone secreting pituitary adenoma causes acromegaly
- symptoms differ from pre-puberty vs post-puberty
- before puberty
- gigantism
- aka increased linear growth
- gigantism
- after puberty
- increased organ size
- increased hand and foot size
- enlargement of tongue
- coarsening of facial features
- insulin resistance and glucose intolerance
- before puberty
- treatment
- GH deficiency
- secretion
- growth hormone
- somatostatin analog (e.g., octreotide)
Posterior Pituitary: Anatomy and Embryology
- posterior pituitary
- posterior pituitary, or neurohypophysis, is the neural portion of the pituitary
- a collection of unmyelinated axons
- axons extend from cell bodies in hypothalamus
- a collection of unmyelinated axons
- consists of pars nervosa, infundibular stalk, and median eminence
- neurophysins carry hormones made in the hypothalamus (ADH and oxytocin) from the hypothalamus to the posterior pituitary
- embryological origin
- neural ectoderm
- posterior pituitary, or neurohypophysis, is the neural portion of the pituitary
- downgrowth of neural ectoderm (diencephalon)
Posterior Pituitary: Hormones
- Antidiuretic hormone (ADH; vasopressin)
- synthesis
- hypothalamic supraoptic nucleus neuronal cell bodies synthesize ADH pro-hormone
- ADH pro-hormone contains ADH and neurophysin II
- ADH pro-hormones are packaged in secretory vesicles
- secretory vesicles are transported via axonal transport to nerve terminals
- nerve terminals in pars nervosa of posterior pituitary
- secretory vesicles are transported via axonal transport to nerve terminals
- ADH pro-hormone processing occurs in secretory vesicles during axonal transport
- cleavage of neurophysin II and release of ADH hormone
- hypothalamic supraoptic nucleus neuronal cell bodies synthesize ADH pro-hormone
- secretion
- action potential depolarizes nerve terminals
- neurosecretory vesicles fuse with plasma membrane
- releases ADH and neurophysin II into perivascular space of highly fenestrated capillaries by which ADH enters systemic circulation
- neurosecretory vesicles fuse with plasma membrane
- action potential depolarizes nerve terminals
- synthesis
- Oxytocin
- synthesis
- neuronal cell bodies of the hypothalamic paraventricular nucleus synthesize oxytocin pro-hormone
- oxytocin pro-hormone contains oxytocin and neurophysin I
- oxytocin pro-hormones are packaged in secretory vesicles
- secretory vesicles are transported via axonal transport to nerve terminals
- nerve terminals in pars nervosa of posterior pituitary
- secretory vesicles are transported via axonal transport to nerve terminals
- oxytocin pro-hormone processing occurs in secretory vesicles during axonal transport
- cleavage of neurophysin I and release of oxytocin hormone
- neuronal cell bodies of the hypothalamic paraventricular nucleus synthesize oxytocin pro-hormone
- secretion
- action potential depolarizes nerve terminals
- neurosecretory vesicles fuse with plasma membrane
- releases oxytocin and neurophysin I into perivascular space of highly fenestrated capillaries by which oxytocin enters systemic circulation
- neurosecretory vesicles fuse with plasma membrane
- action potential depolarizes nerve terminals
- synthesis


