Overview
Snapshot
- A 28-year-old G3P2 female at 39 weeks of gestation is on the labor and delivery floor in active labor. The cervix is 10 centimeters dilated and preparations are made for delivery of the newborn. A male neonate is born with appropriate Apgar scores and without any perinatal complications. During placental delivery there is a lot of resistance when traction is placed on the umbilical cord. After an attempt at manual placental separation, there is profuse bleeding. Obstetric history is significant for previous cesarean delivery. She has missed a number of prenatal visits during this pregnancy.
Introduction
- Overview
- abnormal implantation of the placenta
- Epidemiology
- incidence
- 0.17% prevalence of any placental abnormality during pregnancy
- placenta accreta most common
- 63% of all placental abnormalities
- placenta accreta most common
- 0.17% prevalence of any placental abnormality during pregnancy
- risk factors
- placenta previa (low-lying placenta that covers cervix) after prior C-section
- history of uterine surgery
- advanced maternal age
- multiparity
- history of manual removal of placenta
- infertility procedures
- incidence
- Pathogenesis
- theory of defective decidualization
- thin, poorly formed, partial, absent or dysfunctional decidua in an area of scarring from previous uterine surgery that involved the endometrial-myometrial interface
- allows for placental villi to attach directly to (or invade as in placenta percreta/increta) myometrium
- theory of defective decidualization
- Prognosis
- 27% morbidity
- worse with placenta percreta
- 27% morbidity
- risk of death from sequelae of massive hemorrhage
Classification
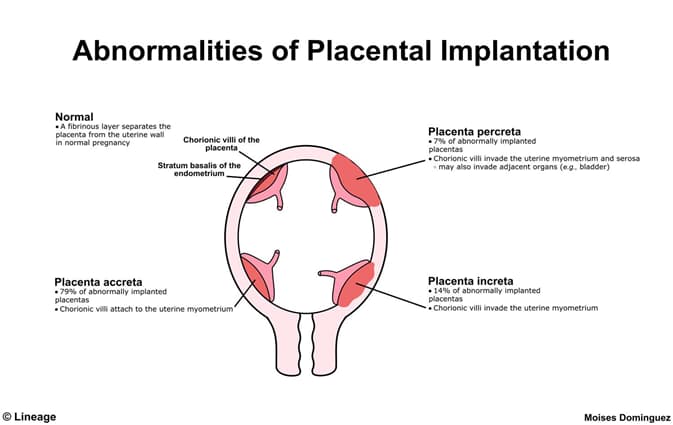
- Placenta accreta spectrum
- placenta accreta
- placental villi attach to myometrium (instead of decidua)
- placenta increta
- placental villi penetrate into the myometrium
- placenta accreta
- placental villi penetrate through the myometrium and attach to the uterine serosa or adjacent organs
Presentation
- Symptoms
- often asymptomatic
- profuse life-threatening hemorrhage during attempted manual placental separation
- Physical Exam
- inability to fully separate placenta from uterus after delivery
Imaging
- Transvaginal or transabdominal ultrasonography
- indications
- routine prenatal care
- a history of cesarean delivery or other uterine surgeries
- used for diagnosis antenatally
- findings
- second and third trimester
- low anterior placenta
- multiple irregularly shaped placental lacunae
- placental lacunae are vascular spaces
- “moth-eaten” appearance of placenta
- myometrial thinning
- placental bulge
- disruption of bladder line
- second and third trimester
- indications
- retroplacental space is disrupted or lost
Studies
- Histology
- placental villi attached to the myometrium in the absence of a decidual plate
- used for diagnosis postnatally
- Maternal serum alpha-fetoprotein
- abnormally elevated in second trimester
Differential
- Placenta increta
- Placenta percreta
- key distinguishing factors
- ultrasound findings
- placental vessels extending through myometrium into bladder or other serosa
- ultrasound findings
- key distinguishing factors
- a focal mass breaking through uterine serosa and extending into bladder
Treatment
- Behavioral
- pre-delivery precautions
- avoidance of sexual intercourse
- avoidance of pelvic exams
- scheduled delivery
- preparation for potential hemorrhage during delivery
- pre-delivery precautions
- Medical
- RhoGAM
- indications
- all Rh(D)-negative mothers with vaginal bleeding if father is Rh(D)-positive or unknown
- modalities
- single intramuscular or intravenous dose
- indications
- blood products
- indications
- massive hemorrhage during delivery
- modalities
- red blood cells
- fresh frozen plasma
- cryoprecipitate
- platelets
- indications
- RhoGAM
- Surgical
- cesarean hysterectomy
- indications
- during delivery to remove adhered placenta
- indications
- cesarean hysterectomy
- typical mode of delivery and treatment for placenta acreta
Complications
- Massive hemorrhage
- Death


