Overview
- Presentation
- Most common complaints are due to mass effects
- e.g., seizures, dementia, focal lesions, headache
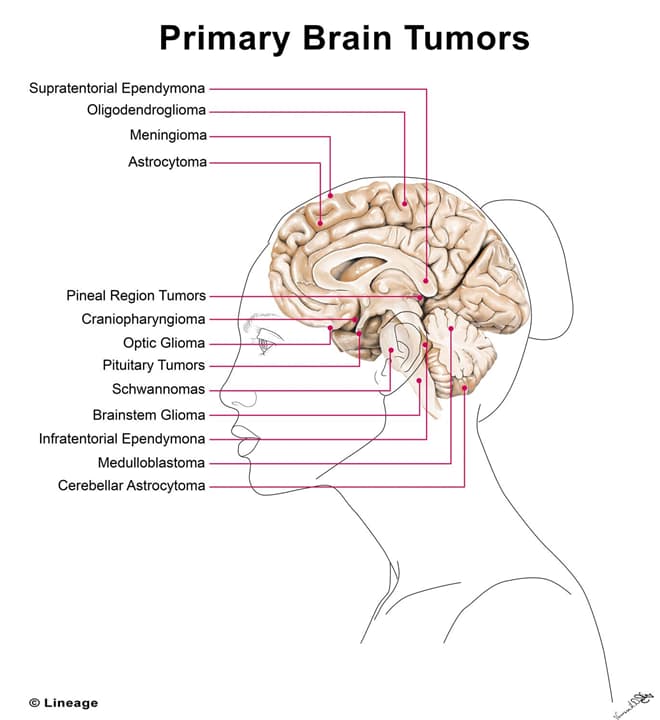
- majority of adult primary tumors are supratentorial
- majority of childhood primary tumors are infratentorial
- Most common complaints are due to mass effects
- Primary tumor characteristics
- rarely undergo metastasis
- usually poorly circumscribed
- primary brain tumor frequency
- meningioma > pituitary tumor > glioblastoma > nerve sheath tumor
- risk factors
- NF, cigarette smoking, Turcot’s syndrome (colonic polyps and brain tumor)
- Secondary tumor characteristics
- 50% of adult brain tumors are due to metastases
- well circumscribed
- frequency of primary tumor causes
- lung > breast > melanoma (skin) > kidney > GI
Adult peak-incidence tumors
- Glioblastoma multiforme
- type: grade IV astrocytoma
- prognosis: grave (< 1 year life expectancy)
- location: cerebral hemispheres
- stain: GFAP
- histologic appearance: “psuedopalisading” pleomorphic tumor cells
- border central areas of necrosis and hemorrhage
- gross appearance: can cross corpus callosum (butterfly glioma)
- Meningioma
- prognosis: resectable
- location: convexities of hemispheres , parasagittal region, olfactory groove
- arises from arachnoid cells covering brain
- histological appearance: spindle cells concentrically arrange in a whorled pattern
- psammoma bodies (laminated calcifications)
- note: more common in women (due to estrogen receptors on tumor cells)
- associated with neurofibromatosis
- Schwannoma
- prognosis: good, resectable
- location: often localized to CN VIII → acoustic schwannoma
- can present with tinnitus, hearing loss
- histologic appearance: biphasic with hypercellular (Antoni A) and hypocellular (Antoni B) areas
- note: bilateral schwannoma found in neurofibromatosis type 2
- Oligodendroglioma
- prognosis: good, slow growing
- location: most often in frontal lobes
- gross appearance: often calcified in frontal lobe
Childhood peak-incidence tumors
- Pilocytic (low-grade) astrocytoma
- type: grade I astrocytoma
- prognosis: benign
- location: most often infratentorial
- may be supratentorial (most commonly, craniopharyngioma)
- stain: GFAP
- gross appearance: cystic + solid, usually well-circumscribed
- Medulloblastoma
- most common malignant intracranial tumor of childhood
- prognosis: poor, highly malignant
- form of primitive neuroectodermal tumor (PNET)
- location: cerebellum
- can compress 4th ventricle → hydrocephalus
- gross appearance: solid
- note: radiosensitive
- Ependymoma
- prognosis: poor
- location: most commonly in 4th ventricle
- can result in hydrocephalus
- can also arise from cauda equina in adults
- Hemangioblastoma (occurs typically in adults if no genetic predisposition as below)
- location: cerebellar
- histologic appearance: foamy cells and high vascularity
- note: associated with von Hippel-Lindau syndrome when found with retinal angiomas
- can produce EPO → secondary polycythemia
- Craniopharyngioma
- prognosis: benign
- location: near sella turcica
- can present with optic chiasm compression → bitemporal hemianopia
- confused with pituitary adenoma
- can present with optic chiasm compression → bitemporal hemianopia
- gross appearance: calcification is common, tooth enamel-like
- Germinoma
- prognosis: good
- location: pineal gland and suprasellar region
- derived from nests of embryonic cells arrested during their migration in fetal development
- Pineal region: Parinaud syndrome (30-40% of cases) compression of tectum causes: paralysis of upward gaze, loss of light perception and accomodation, nystagmus, failure of convergence
- Suprasellar region: anterior hypopituitarism, precocious puberty, diabetes inspidius, visual disturbances
- stain: AFP and b-HCG


