Overview
Introduction
- Basic principle
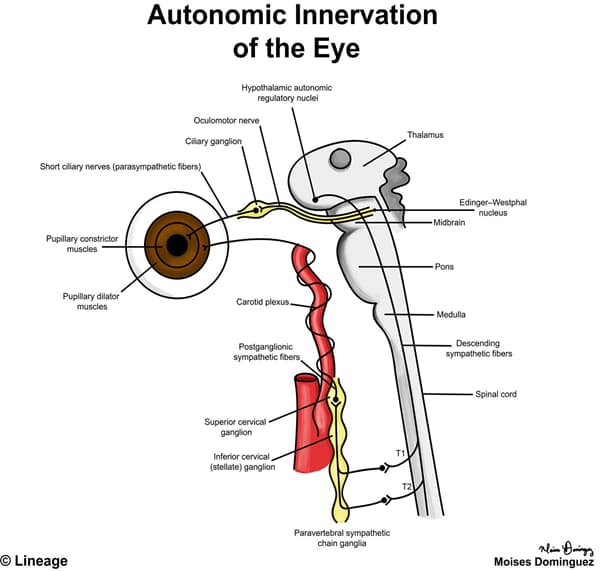
- the parasympathetic and sympathetic nervous system control the pupil
- parasympathetic fibers lead to pupillary constriction (miosis)
- sympathetic fibers lead to pupillary dilation (mydriasis)
- as well as controlling the
- superior tarsal muscle
- elevates the upper lid
- smooth muscle orbitalis
- prevents eye sinking into the orbit
- facial and neck cutaneous arteries and sweat glands
- superior tarsal muscle
- as well as controlling the
- the parasympathetic and sympathetic nervous system control the pupil
- Miosis
- light enters the eye which activates
- retinal ganglion cells that will project axons into the optic nerve → optic chiasm → optic tract and then reach the
- pretectal nucleus
- retinal ganglion cells that will project axons into the optic nerve → optic chiasm → optic tract and then reach the
- fibers from the pretectal nucleus project to the Edinger-Westphal nucleus
- pre-ganglionic parasympathetic fibers exit the Edinger-Westphal nucleus and synapse in the
- ciliary ganglion
- pre-ganglionic parasympathetic fibers exit the Edinger-Westphal nucleus and synapse in the
- light enters the eye which activates
- Mydriasis
- sympathetic fibers from many hypothalamic nuclei descend and reach T1 and T2 spinal cord levels
- pre-ganglionic sympathetic fibers exit the T1 and T2 spinal cord level to join the paravertebral sympathetic chain (via the white ramus) and
- synapse to the superior cervical ganglion
- pre-ganglionic sympathetic fibers exit the T1 and T2 spinal cord level to join the paravertebral sympathetic chain (via the white ramus) and
- post-ganglionic sympathetic fibers ascend via the carotid plexus of the internal carotid artery, goes through the cavernous sinus, and synapses to the
- pupillary dilator muscle
- sympathetic fibers from many hypothalamic nuclei descend and reach T1 and T2 spinal cord levels
| Select Pupillary Defects | |
| Pupillary Defect | Comments |
| Horner syndrome | Pathogenesis inolves impairment in sympathetic pathways to the eye and face which results inptosissecondary to impaired innervation into the upper lid smooth musclesmiosissecondary to impaired innervation into the pupillary dilator musclesanhidrosis |
| Marcus Gunn pupil | Describes an afferent pupillary defect resulting inthe affected eye is not sensitive to the lightthere is minimal or absent pupillary constriction of the affected eye to lightA lesion may affecteyeretinaoptic nerveAfferent pupillary defects can be detected withswinging flashlight test which will showthe affected pupil dilate when exposed to the penlight |
| Argyll Robertson pupil | A type of light-near dissociation wherethe eye does not constrict in response to light as much as it does with accomodationAssociated with neurosyphilis |
| Adie’s myotonic pupil | A type of light-near dissociation wherethe eye does not constrict in response to light as much as it does with accomodationSecondary todegeneration of theciliary ganglionpostganglionic parasympathetic neurons |



