Overview
Introduction
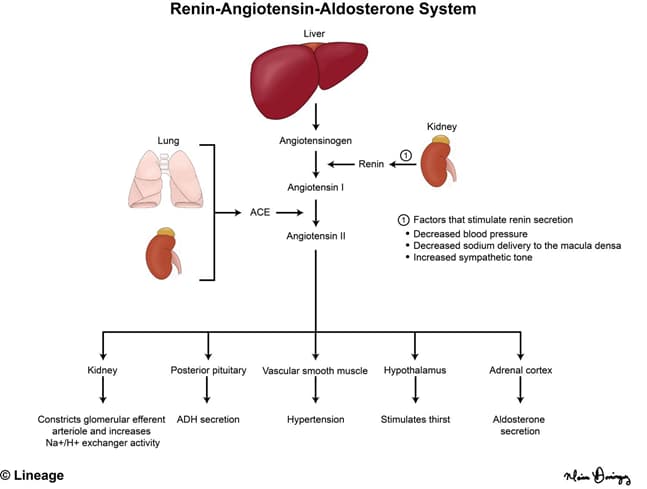
- The renin-angiotensin-aldosterone system (RAAS) attempts to maintain arterial blood pressure by controlling blood volume
- a decrease in arterial blood pressure is sensed by the kidneys as decreased renal perfusion pressure
- this in turn stimulates the juxtaglomerular cells to secrete renin into circulation
- note that increased sympathetic activity and β1-agonists (e.g., isoproterenol) increase renin secretion
- note that a decrease in Na+ delivery to the macula densa also stimulates RAAS
- this in turn stimulates the juxtaglomerular cells to secrete renin into circulation
- angiotensin II activates type I G protein-coupled angiotensin II receptors (AT1) receptors which
- acts on the adrenal cortex (zona glomerulosa) to increase aldosterone secretion
- directly stimulates the Na+-H+ exchange
- acts on the hypothalamus to increase thirst and the pituitary to increase anti-diuretic hormone (ADH) secretion
- ADH will act on the principal cells to increase aquaporin-2 expression
- this increases the collecting duct’s permeability to water and thus increases water reabsorption
- ADH will act on the principal cells to increase aquaporin-2 expression
- acts on arterioles to increase total peripheral resistance and thus increasing arterial pressure
- preferrentially constricts the efferent arteriole to maintain glomerular filtration rate (GFR) in low volume states (e.g., hemorrhaging)
- a decrease in arterial blood pressure is sensed by the kidneys as decreased renal perfusion pressure


