Snapshot
- A 25-year-old African American woman presents to her dermatologist for a bothersome scar. She reports that a few months ago, she injured her arm after falling off a bike. Since then, her cut has healed and a raise flesh-colored scar has grown over the wound. It is often itchy or even painful. On physical exam, she has a 7 cm raised scar with irregular borders that extends beyond the original wound. (Keloid)
Overview
- Skin is the largest organ of the body
- Functions
- photoprotection
- barrier formation
- homeostasis
- thermoregulation
- immunologic protection
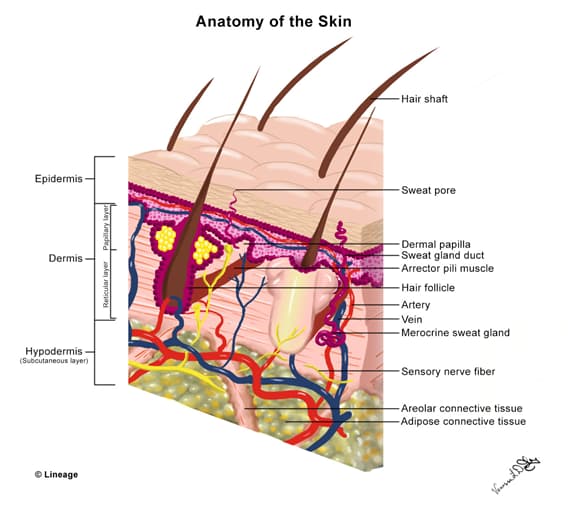
- Skin is made of the epidermis and dermis
Anatomy
- Epidermis
- layers from top to bottom
- stratum Corneum
- serves as a physiologic barrier from
- chemical and microbiologic invasion
- fluid and solute loss
- serves as a physiologic barrier from
- stratum Lucidum
- stratum Granulosum
- stratum Spinosum
- stratum Basale
- separates the epidermis and dermis
- “Californians Like Girls in String Bikinis”
- stratum Corneum
- major cells
- keratinocytes
- mature from the stratum basale to the stratum corneum over the course of 4 weeks
- melanocytes
- produces melanin, which protects the skin from ultraviolet radiation
- Langerhan cells
- immune cells that present antigens
- Merkel cells
- contain neuroendocrine peptides
- keratinocytes
- layers from top to bottom
- Dermis
- layers from top to bottom
- papillary dermis
- reticular dermis
- functions as structural support and provides nutrition via the vasculature
- layers from top to bottom
- nerves
Normal Wound Healing
- Wound disrupts structure and function of epidermis
- Activates keratinocytes, fibroblasts, endothelial cells, platelets, and macrophages
- Hemostasis and inflammatory phase (0-3 days)
- clot forms with platelet aggregation, trigger of clotting cascade, and small vessel constriction
- mast cells release histamine and other vasodilators to increase permeability in vasculature
- neutrophils and other inflammatory cells migrate into tissue
- edema or swelling is seen clinically
- macrophages clear debris
- Proliferative phase (3 days to weeks)
- fibroblasts
- deposits glycoprotein and mucopolysaccharides
- produce myofibroblasts
- myofibroblasts help to contract the wound to pull the edges together
- synthesize collagen (type III)
- the resulting collagen matrix stimulates angiogenesis
- the resulting collagen deposition and angiogenesis form granulation tissue
- abnormal wound healing in this phase
- deficiency in vitamin C or copper can result in delayed wound healing
- keloids and hypertrophic scars may result from persistent myofibroblasts or excessive matrix synthesis
- fibroblasts
- Remodeling (weeks to months)
- type III collagen is replaced by type I collagen, resulting in increased tensile strength of the tissue
- vessels mature
- remodeling is mediated by fibroblasts
- abnormal wound healing in this phase
- deficiency in zinc can result in delayed wound healing
Wound Closure Intentions
- Primary intention
- wound edges are re-approximated
- faster healing and less scarring
- Secondary intention
- wounds are left open and allowed to granulate and fill in over time
- Tertiary intention (delayed closure)
- wounds are left open and observed
- wounds are then approximated and closed later


