Introduction
- Major histocompatibility complexes (MHC) are cell surface expressed proteins that
- bind to protein peptides in a surface groove
- present bound peptides to
- receptors on circulating T-cells
- participate in the
- activation of the adaptive immune response
- MHC are encoded by HLA genes that are localized to several different genetic regions
- different HLA regions encode for different types of MHC
- Allogenic MHC can be recognized by T-cells of the adaptive immune system
- mismatch of MHC is an important cause of transplant rejection
MHC Classes
- There are two different classes of MHC encoded in the human genome
- class I MHC usually presents
- endogenous antigens to CD8+ killer T-cells
- class II MHC usually presents
- endocytosed antigens to CD4+ helper T-cells
- antigens may be “cross-presented” by the other MHC class in some cases
- class I MHC usually presents
- The two MHC classes differ in several characteristics including
- HLA loci that encodes the gene
- sites of expression
- protein structure
- antigen loading site
- antigen loading mechanism
- binding partners
· Each individual possesses a set of MHC class I and class II subtypes
o these “haplotypes” define the peptides that will be recognized
· Some haplotypes are associated with specific diseases because they may
o preferentially bind to certain self-peptides
lead to a failure of immune tolerance
Major Histocompatibility Complex (MHC), also known as Human Leukocyte Antigen (HLA) in humans, plays a critical role in the immune system’s recognition of self and non-self antigens. MHC molecules are essential for presenting antigens to T cells, which initiates an immune response. Understanding the structure and function of MHC is crucial for medical professionals, especially those in immunology, transplantation, and infectious diseases. This article provides a comprehensive overview of the structure, types, function, related studies, treatment considerations, and clinical significance of MHC.
Structure of MHC:
Major Histocompatibility Complex molecules are glycoproteins located on the surface of nearly all nucleated cells in vertebrates. They can be divided into two main classes:
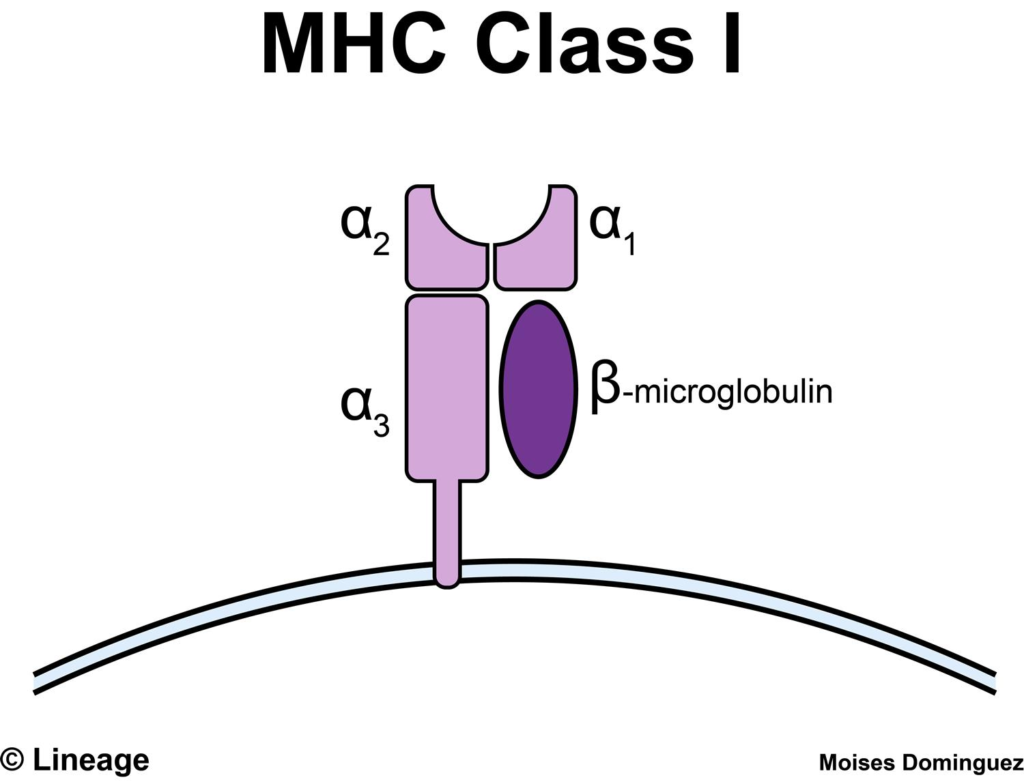
- MHC Class I Molecules: MHC class I molecules are expressed on the surface of all nucleated cells and are responsible for presenting intracellular antigens to CD8+ T cells (cytotoxic T cells). They consist of a heavy chain (alpha chain) and a small non-covalently associated protein called β2-microglobulin.
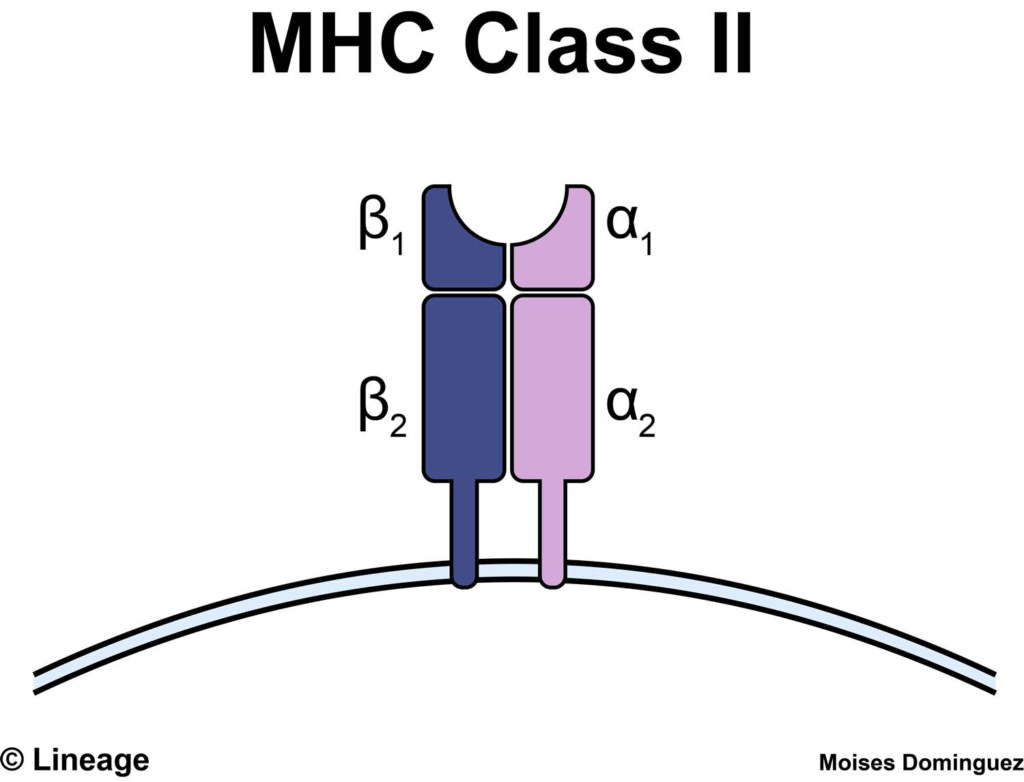
- MHC Class II Molecules: MHC class II molecules are primarily expressed on antigen-presenting cells (APCs), such as dendritic cells, macrophages, and B cells. They present extracellular antigens to CD4+ T cells (helper T cells). MHC class II molecules consist of two chains, an alpha chain, and a beta chain.
Function of Major Histocompatibility Complex:
The primary function of MHC is to present antigens to T cells, initiating an immune response. This process involves the following steps:
- Antigen Processing: Intracellular antigens, such as viral or tumor antigens, are processed in the cytoplasm by the proteasome into small peptides. Extracellular antigens are taken up by APCs, processed within endosomes, and also converted into small peptides.
- Antigen Presentation: MHC class I molecules present the intracellular peptides to CD8+ T cells, while MHC class II molecules present extracellular peptides to CD4+ T cells.
- T Cell Activation: The T cell receptor (TCR) on the surface of CD8+ or CD4+ T cells recognizes the antigen-MHC complex, leading to T cell activation. This activation triggers an immune response, leading to the elimination of infected or abnormal cells.
Major Histocompatibility Complex Types:
- MHC Polymorphism: MHC molecules are highly polymorphic, meaning there are many different MHC alleles within a population. This diversity allows the immune system to recognize a wide range of antigens.
- MHC Haplotypes: Each individual inherits a set of MHC genes from each parent, creating a unique combination known as an MHC haplotype. MHC haplotypes influence the individual’s immune response and ability to present and recognize antigens.
Clinical Significance:
- Transplantation: Major Histocompatibility Complex plays a crucial role in organ transplantation. The compatibility of MHC between the donor and recipient is essential to prevent graft rejection. The closer the MHC match, the lower the risk of rejection.
- Autoimmune Diseases: Dysregulation of MHC presentation can contribute to the development of autoimmune diseases, where the immune system attacks the body’s own tissues.
Major Histocompatibility Complex Studies:
- Genetic Studies: Genetic studies focus on identifying specific MHC alleles associated with certain diseases or immune responses.
- Immunological Studies: Immunological studies investigate the interactions between MHC molecules, antigens, and T cell receptors to understand immune responses better.
Treatment Considerations:
- Transplantation: Matching the Major Histocompatibility Complex between the donor and recipient is critical for successful organ transplantation. Immunosuppressive medications may also be used to prevent graft rejection.
- Autoimmune Diseases: Treatments for autoimmune diseases often target the immune system to reduce inflammation and suppress the immune response against self-antigens.
Conclusion:
Major Histocompatibility Complex is a crucial component of the immune system, responsible for presenting antigens to T cells, initiating immune responses, and regulating self and non-self recognition. MHC class I molecules present intracellular antigens to CD8+ T cells, while Major Histocompatibility Complex class II molecules present extracellular antigens to CD4+ T cells. MHC polymorphism and haplotypes contribute to individual variations in immune responses.
In transplantation, matching MHC between the donor and recipient is essential to prevent graft rejection. Dysregulation of MHC presentation can also contribute to autoimmune diseases. Ongoing research in MHC genetics, immunology, and transplantation continues to enhance our understanding of MHC’s structure and function and its clinical significance, leading to improved treatments and outcomes in various immune-related conditions.



