Direct Sympathomimetics
Indirect Sympathomimetics
Overview
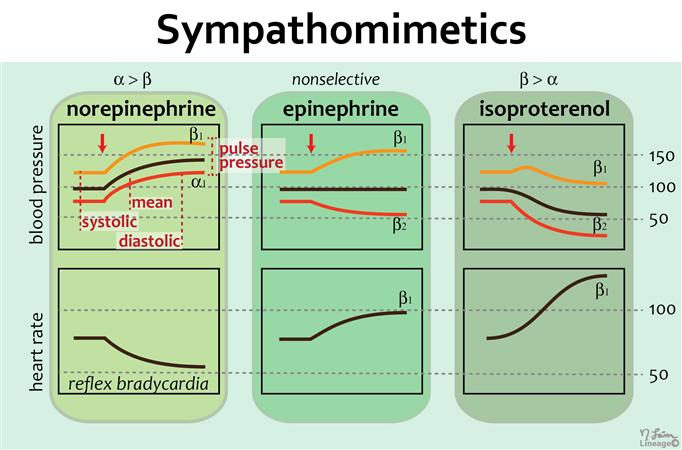
Sympathomimetics are a class of drugs that mimic or stimulate the effects of the sympathetic nervous system, which is responsible for the body’s “fight-or-flight” response. They primarily act on adrenergic receptors, which are found throughout the body and play a role in various physiological processes. Here’s an overview of sympathomimetics:
- Mechanism of action: Sympathomimetics work by binding to adrenergic receptors and activating them, leading to increased stimulation of the sympathetic nervous system. They can mimic the effects of natural neurotransmitters such as norepinephrine and epinephrine (adrenaline).
- Indications: Sympathomimetics have a wide range of clinical uses due to their effects on different organ systems. Some common indications for sympathomimetics include the treatment of asthma, nasal congestion, hypotension (low blood pressure), bradycardia (slow heart rate), anaphylaxis (severe allergic reaction), and attention deficit hyperactivity disorder (ADHD).
- Types of sympathomimetics: a. Catecholamines: Catecholamines are a class of sympathomimetics that include naturally occurring compounds like epinephrine, norepinephrine, and dopamine. They have a short duration of action and are typically administered through injection. b. Non-catecholamines: Non-catecholamine sympathomimetics, such as albuterol and phenylephrine, have a longer duration of action and can often be administered orally, topically, or by inhalation.
- Adverse effects: Sympathomimetics can produce various side effects, which can vary depending on the specific drug and its target receptors. Common side effects include increased heart rate, elevated blood pressure, palpitations, restlessness, anxiety, tremors, sweating, headache, and gastrointestinal disturbances. Higher doses or excessive use can lead to more severe effects, including arrhythmias, myocardial infarction, stroke, and hypertensive crisis.
- Contraindications and precautions: Sympathomimetics are contraindicated in individuals with certain conditions, such as uncontrolled hypertension, coronary artery disease, arrhythmias, hyperthyroidism, and closed-angle glaucoma. They should be used with caution in patients with pre-existing cardiovascular or cerebrovascular diseases, diabetes, hyperthyroidism, and anxiety disorders.
- Drug interactions: Sympathomimetics may interact with other medications, such as monoamine oxidase inhibitors (MAOIs), beta-blockers, and certain antidepressants, potentially leading to adverse effects or reduced efficacy. It’s important to inform healthcare providers about all medications being taken to minimize the risk of interactions.
As sympathomimetics can have significant cardiovascular effects, their use should be closely monitored by healthcare professionals. Dosage adjustments and careful consideration of individual patient factors are necessary to ensure the safe and effective use of sympathomimetic medications.
Studies
Sympathomimetics have been extensively studied in various areas of medicine and pharmacology. Here are some notable areas of research and studies related to sympathomimetics:
- Asthma and respiratory conditions: Sympathomimetics such as beta-agonists (e.g., albuterol) are commonly used as bronchodilators to treat asthma and other respiratory conditions. Numerous studies have focused on their efficacy and safety in relieving bronchospasm and improving respiratory symptoms.
- Cardiovascular conditions: Sympathomimetics have been studied in the management of cardiovascular conditions like hypotension, bradycardia, and heart failure. Research has examined their effects on increasing blood pressure, heart rate, and cardiac output, as well as their potential benefits in acute settings or as long-term therapy.
- Attention deficit hyperactivity disorder (ADHD): Stimulant sympathomimetic medications, such as methylphenidate and amphetamines, are commonly prescribed for the treatment of ADHD. Studies have investigated their effectiveness in reducing ADHD symptoms, improving cognitive function, and assessing their long-term safety and potential risks.
- Nasal congestion: Sympathomimetics, including decongestant agents like phenylephrine and pseudoephedrine, are used to alleviate nasal congestion. Research has focused on their efficacy in relieving nasal congestion and potential adverse effects, particularly regarding rebound congestion with prolonged use.
- Anaphylaxis and allergic reactions: Epinephrine, a potent sympathomimetic, is the drug of choice for treating severe allergic reactions, including anaphylaxis. Numerous studies have evaluated the effectiveness of epinephrine in reversing allergic symptoms, preventing further complications, and optimizing the management of anaphylactic emergencies.
- Neurological conditions: Some sympathomimetics, such as dopaminergic agents, have been studied in the treatment of neurological conditions like Parkinson’s disease and attention disorders. Research has explored their impact on dopamine regulation, motor symptoms, and cognitive function.
- Drug development and optimization: Ongoing research aims to develop new sympathomimetic drugs with improved selectivity, reduced side effects, and enhanced therapeutic efficacy. These studies focus on understanding the structure-activity relationships and receptor interactions to design more specific and targeted sympathomimetic agents.
Check out USMLE Step 1 Mastery: Comprehensive Course and Lecture Notes.


