Overview
Snapshot
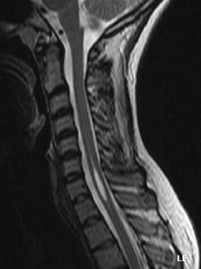
- A 32-year-old man presents with bilateral upper extremity weakness and sensory loss. Approximately 6 months ago, he was involved in a motor vehicle accident. On physical exam, skin ulcerations are noted on the ventral aspect of the hands. There is preservation of light touch, vibration and proprioception in the upper extremity bilaterally. MRI of the cervical spinal cord is shown.
Introduction
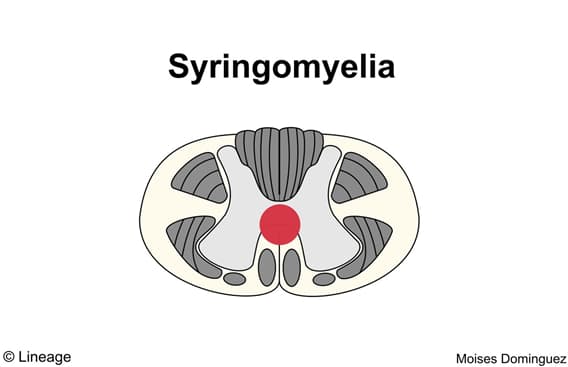
- Cavitation within the spinal cord that damages surrounding spinal tracts
- damage to anterior white commissure of spinothalamic tract
- “cape-like” deficit in pain and temperature
- preserves proprioception and vibration sense (dorsal columns)
- cavitation expansion can compress ventral horn motor neurons
- bilateral flaccid paralysis
- may involve descending hypothalamic fibers to preganglionic sympathetic neurons of T1-T4
- Horner’s syndrome
- damage to anterior white commissure of spinothalamic tract
- Associated conditions
- Arnold-Chiari malformation
- spinal trauma
- malignancy
- Epidemiology
- male > women
- 30 – 40 years old
Presentation
- Symptoms
- bilateral loss of pain and temperature sensation
- muscle atrophy/weakness
- if anterior motor horns involved
- these run close to the lateral spinothalamic tracts in the medulla
Evaluation
- MRI
- syrinx cavity can be seen
- should rule-out chiari malformation if syrinx cavity is noted
Differential
- Spinal epidural abscess
- Diabetic neuropathy
- Acute inflammatory demyelinating polyradiculoneuropathy (AIDP)
Treatment
- Surgical
- posttraumatic
- decompression if indicated
- surgically correct underlying condition
- posttraumatic
- e.g., posterior fossa decompression in chiari I malformation
Prognosis, Prevention, Complications
- Prognosis
- dependent on etiology and severity
- Complications
- neuropathic pain
- bulbar symptoms in patients with syringobulbia



