Overview
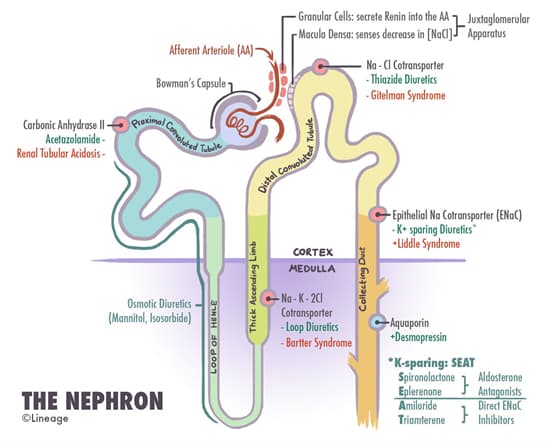
Proximal Convoluted Tubule
- The major function of the proximal convoluted tubule (PCT) is
- isosmotic reabsorption of solutes and water which is imperative for maintaining the extracellular fluid (ECF)
- this is accomplished by a number of co-transporters such as
- Na+-glucose co-transporter (SGLT)
- 100% of the filtered glucose is reabsorbed
- Na+-amino acid co-transporter
- 100% of the filtered amino acids are reabsorbed
- Na+-phosphate co-transporter
- Na+-H+ exchange
- Na+-glucose co-transporter (SGLT)
- this is accomplished by a number of co-transporters such as
- isosmotic reabsorption of solutes and water which is imperative for maintaining the extracellular fluid (ECF)
- Note that the PCT can be divided into an early and late PCT
- Na+ is reabsorbed in both portions of the PCT but via different mechanisms
- early PCT
- Na+ is primarily reabsorbed with HCO3–
- 85% of the filtered HCO3– is reabsorbed
- Na+ is also reabsorbed with glucose, amino acids, and other organic solutes (e.g., lactate and citrate)
- Na+ is primarily reabsorbed with HCO3–
- late PCT
- Na+ is primarily reabsorbed with Cl–
- early PCT
- Na+ is reabsorbed in both portions of the PCT but via different mechanisms
- There are a number of hormones that act on the PCT and they include
- angiotensin II
- stimultes the Na+-H+ exchange
- angiotensin II
- Medications that act on this portion of the nephrone includes
- carbonic anhydrase inhibitors (e.g., acetazolamide)
- osmotic diuretics (e.g., mannitol)
Thin Descending Loop of Henle
- The thin descending loop of Henle is permeable to water but not ions
- water moves out of the loop into the interstitium resulting in the tubular fluid becoming more concentrated (hyperosmotic)
Thick Ascending Loop of Henle
- The major function of the thick ascending loop of Henle is to reabsorb NaCl without water
- There is also paracellular reabsorption of Ca2+ and Mg2+
- this is driven by the lumen-positive potential difference generated by K+ backleak
Distal Convoluted Tubule and Collecting Duct
- The distal convoluted tubule (DCT) can be divided into an early and late DCT
- early DCT
- reabsorbs 5% of the filtered sodium via a Na+-Cl− cotransporter
- this is the site of action of thiazide (e.g., hydrochlorothiazide and metolazone) diuretics
- thiazides are organic acids that bind to the Cl− site of the transporter
- this is the site of action of thiazide (e.g., hydrochlorothiazide and metolazone) diuretics
- it is impermeable to water and thus dilutes the tubular fluid (thus called the cortical diluting segment)
- reabsorbs 5% of the filtered sodium via a Na+-Cl− cotransporter
- late DCT and collecting duct
- both of these segments of the nephron are anatomically and functionally similar
- there are 2 major cell types
- principal cells
- Na+ is reabsorbed via epithelial Na+ channels (ENaC)
- K+-sparing diuretics (e.g., spironolactone, amiloride, and triamterene) impair Na+ reabsorption
- spironolactone is an aldosterone antagonist
- amiloride and triamterene act at the level of Na+ channels
- K+-sparing diuretics (e.g., spironolactone, amiloride, and triamterene) impair Na+ reabsorption
- anti-diuretic hormone (ADH) increases water permeability of the principal cells
- this is accomplished by binding to V2 receptors and subsequently resulting in increased aquaporin-2 (AQP2) channel expression
- there is a Ca2+-Na+ exchange in the basolateral membrane of the principle cell
- PTH increases Ca2+ reabsorption by increase exchange activity
- Na+ is reabsorbed via epithelial Na+ channels (ENaC)
- α-intercalated cells
- secretion of H+ is accomplished by 2 active transport mechanisms
- H+-ATPase
- this enzyme is stimulated by aldosterone
- H+-K+ ATPase
- H+ is secreted in exchange for K+
- H+-ATPase
- secretion of H+ is accomplished by 2 active transport mechanisms
- principal cells
- early DCT



